Method Article
Treatment Model for Young Patients with Psychogenic Erectile Dysfunction and Resultant Infertility
* Wspomniani autorzy wnieśli do projektu równy wkład.
W tym Artykule
Podsumowanie
An integrated treatment model for unconsummated marriage (UCM) due to psychogenic erectile dysfunction is presented, offering streamlined management from assessment to intervention. Emphasizing patient-centered care and communication, preliminary results show improved success rates and satisfaction, supporting its effectiveness in addressing infertility in UCM from the male perspective.
Streszczenie
Conventional management of erectile dysfunction (ED)-related non-consummation and infertility often overlooks psychosocial determinants and dyadic involvement, leading to suboptimal therapeutic outcomes, including persistent sexual dysfunction and reduced couple satisfaction. This study proposes and validates a novel, patient-centric intervention tailored for young individuals with psychogenic ED (pED), targeting both erectile recovery and infertility resolution. The "Streamlined Clinical Process" incorporates structured treatment strategies for both the patient and their partner, including evidence-based sexual health education, psychological support, partner-inclusive counseling, sensate focus training, lifestyle modification, on-demand pharmacotherapy, and structured follow-up. Following comprehensive baseline assessments (medical history, physical examination, and diagnostics), the treatment team collaboratively formulates individualized 16-week regimens with active partner engagement. Three key innovations distinguish this protocol: (1) The implementation of the GLTC (Goodwill-Listening-Talking-Cooperation) communication framework, which addresses patients' psychological needs and promotes effective communication strategies; (2) The application of Hawton's psychosexual stratification to identify specific psychological factors, with the aim of reshaping negative sexual beliefs, alleviating anxiety, improving sexual function, and rebuilding mutual trust and emotional connection between partners; (3) The development of easy-to-understand videos for psychological education to enhance treatment adherence through iterative patient-provider dialogue. Results demonstrate clinically meaningful improvements in erectile function recovery rates, coital success frequency, and couple satisfaction. Notable challenges include patient adherence to the treatment plan and the timely effectiveness of non-pharmacological interventions. In conclusion, this model presents a scalable and effective strategy for addressing sexual dysfunction-related infertility in young patients, offering a valuable framework for clinical practice and future research in sexual medicine.
Wprowadzenie
Erectile dysfunction (ED), defined as the persistent inability to attain or sustain an erection adequate for satisfactory sexual performance, is predominantly associated with psychological factors -- termed psychogenic erectile dysfunction (pED) -- which account for 85%-90% of cases1,2. Although ED may result from vascular disease, hormonal dysregulation, or neurological impairments, pED is characterized by the absence of significant organic abnormalities. Instead, its etiology involves factors such as anxiety, depressive disorders, chronic stress, or adverse sexual experiences that interfere with the neurovascular mechanisms required for erectile function.
Notably, pED disproportionately affects individuals under the age of 403, a demographic that experiences elevated anxiety levels due to psychosocial stressors. A subset of patients presents with persistent sexual dysfunction beginning at the time of marriage or cohabitation, clinically referred to as unconsummated marriage (UCM) or "honeymoon-phase ED"4,5. The prevalence of UCM in male outpatient clinics ranges from 4% to 17%, with variability influenced by cultural norms (e.g., stigmatization of premarital sexual health education), diagnostic heterogeneity, healthcare access limitations, and cohort selection biases.
Anxiety disorders are present in 74.4% of UCM cases, with pED identified as the principal etiological factor in affected males6,7. Post-cohabitation infertility affects 65% of UCM couples. Consultation for infertility often occurs under pressure from familial expectations (e.g., intergenerational desire for offspring) and societal stigma (e.g., cultural taboos surrounding male sexual health). These sociocultural dynamics contribute to delayed treatment-seeking behavior, driven by fear of social judgment and internalized stress related to nonconformity with normative gender roles, as reported at the 2019 Joint Meeting of the International Society for Sexual Medicine8.
In clinical practice, patients with pED frequently present with performance anxiety or fear of failure during consultations. However, these concerns are often attributed solely to physical causes, with minimal exploration of underlying psychological triggers. For instance, a common clinical scenario involves prescribing phosphodiesterase-5 (PDE5) inhibitors without evaluating psychosocial comorbidities such as relationship discord or a history of sexual trauma. This may be due to a traditional lack of awareness, knowledge, and training among urologists and andrologists in assessing key psychological factors related to ED9. Furthermore, cultural and economic disparities across regions pose additional challenges in addressing these issues10. Major barriers include prolonged patient communication requirements that overwhelm physicians with limited communication skills, a lack of sexual health and psychological education for patients, compounded by the absence of appropriate billing codes to reflect the physician's effort; and the lack of collaborative psychosocial therapy teams or consultation services.
Typically, patients seek treatment from urology or andrology clinics that focus primarily on male factors, rather than on the couple as a unit. As a result, treatment is often narrowly focused on symptom management -- specifically, the administration of PDE5 inhibitors to improve erection hardness and increase the success rate of intercourse11. While this method proves effective for some, it is insufficient for many, as it overlooks the psychological and relational factors critical to patients with pED. These neglected aspects include managing performance anxiety, improving sexual communication between partners, and addressing the emotional impact of repeated sexual failures.
A more holistic approach is essential for long-term treatment success. The limitations of the conventional approach become increasingly evident with a growing number of consulting couples. Problems often arise when patients discontinue PDE5 inhibitor use, resulting in recurrent failures in consummating marriage and growing distrust in the treatment plan. Additionally, unresolved issues of low male self-esteem contribute to new psychological difficulties12,13, including reliance on medication for sexual performance. Ultimately, these approaches fail to resolve natural conception challenges faced by the couple and may give rise to more complex problems. These include emotional distress such as depression and anxiety from repeated treatment failures, marital strain, family conflicts, societal pressure to bear children, and the stigmatization of infertility.
These challenges necessitate a reevaluation of the psychopathological dimensions within clinical frameworks. Hawton's etiological classification stratifies contributing factors into predisposing, precipitating, and perpetuating elements14,15, which frequently exhibit comorbidity16. Under the influence of these factors, patients often experience emotional instability, such as anxiety and strained interpersonal relationships. Their emotions are highly sensitive to the manner of communication. The physician's communication style plays a critical role in gaining the patient's cooperation and trust in the treatment process. Similarly, effective patient sex education and psychological counseling aimed at fostering medical cooperation depend heavily on the healthcare provider's communication skills. Affective dysregulation -- manifesting as anxiety disorders and interpersonal conflict -- typically emerges under these psychodynamic influences. Crucially, patients' emotional states are highly susceptible to clinician communication styles, which fundamentally influence the formation of a therapeutic alliance and adherence to treatment. This interdependence also affects the efficacy of psychosexual education and medical collaboration, both of which rely on the communicative competence of healthcare professionals.
The GLTC (Goodwill-Listening-Talking-Cooperation) framework, through its systematic integration of biomedical protocols and humanistic engagement, demonstrates strong cultural adaptability17,18. This framework emphasizes improving physicians' listening skills and enhancing verbal communication techniques. By attentively listening to patients and offering timely feedback, physicians can better understand patient needs and build trust. Additionally, using friendly body language, warm verbal expressions, and encouraging dialogue helps foster patient trust, thereby improving the doctor-patient relationship and elevating the quality of care18,19,20.
This approach is particularly important in treating patients with psychogenic sexual dysfunction. It is recommended that the GLTC communication framework be integrated throughout the entire treatment process, with implementation plans tailored to individual patient differences17,21. This is especially relevant in the context of andrological therapy. To address the clinical challenges faced by young couples experiencing infertility due to psychogenic ED, a diagnostic and treatment model has been developed that integrates Hawton's classification method15 with the GLTC communication framework, resulting in notable outcomes.
Protokół
All procedures described below were reviewed and approved by the Institutional Review Board of the Affiliated Panyu Central Hospital of Guangzhou Medical University, under trial registration number ChiCTR1800019279. At the initial consultation beginning in June 2020, participants provided informed consent after receiving a thorough explanation of the treatment purpose, procedures, and data handling protocols. It was ensured that all information would remain confidential and be used exclusively for research purposes. Discussions involving sexual health education and personal histories were conducted privately and with the utmost sensitivity. All interactions were carried out respectfully, with the dignity of each participant preserved. Personal identifiers were removed, and unique codes were assigned to anonymize participant data, which was securely stored on encrypted, password-protected systems and in locked cabinets to prevent identity linkage and unauthorized access. Details of the reagents and equipment used are listed in the Table of Materials.
1. Patient selection
- Set the inclusion criteria
- Select men aged 18-40 who have been unable to complete intercourse despite at least two attempts5, and who have been unable to achieve pregnancy after one year of regular, unprotected intercourse.
- Select patients with a score <22 on the International Index of Erectile Function (IIEF-5) (Supplementary Table 1).
- Ensure that patients exhibit psychological factors as determined by the Hawton classification15 (Supplementary Table 2 and Supplementary Table 3).
- Ensure that patients have normal secondary sexual characteristics.
- Ensure that patients are married or in a stable sexual relationship and are capable of engaging in at least one normal intercourse per week from the start to the completion of the study.
- Ensure that the female partner does not have significant sexual dysfunction or other factors contributing to the failure to consummate the marriage due to lack of sexual knowledge.
- Ensure that patients have not used any erectile dysfunction medications or other drugs intended to improve erectile function within four weeks prior to treatment.
- Set the exclusion criteria22
- Exclude patients with secondary ED resulting from vascular, endocrine, or medication-induced causes.
- Exclude patients with psychiatric disorders caused by schizophrenia or severe mood disorders.
- Exclude patients with significant neurological damage or anatomical genital abnormalities.
- Exclude patients with severe cardiovascular or cerebrovascular diseases.
- Exclude patients with a history of substance abuse, including drug or alcohol dependency.
- Exclude patients currently receiving ongoing medical treatments, such as chronic pain management or therapies for autoimmune diseases.
2. Layout of the andrology area
- Waiting area
- Establish a waiting area at the point of registration. Ensure that a guide nurse assesses the patient's needs and introduces the functions of various sections, along with the basic consultation process (see Figure 1A).
- Form-filling area
- Set up a form-filling area. Ensure that patients complete a self-designed erectile dysfunction history questionnaire, including details on onset time, current sexual frequency, marital and reproductive history, masturbation habits, and treatment history.
- Include standardized assessment scales such as the International Index of Erectile Function (IIEF-5)23 and the International Premature Ejaculation Diagnostic Tool (PEDT)24 before the consultation (see Figure 1A).
- Clinic area
- Establish a clinic area consisting of seven independent rooms (see Figure 1A,B).
- Set up two andrology consulting rooms. Ensure that physicians working in these rooms are trained in GLTC communication skills.
- Set up one health consultation room. Ensure that nurses assigned to this room are also trained in GLTC communication skills.
- Set up an educational room. Equip this room with sexual and psychological health literature/videos, anatomical models of reproductive organs, and penis erection hardness models.
- Set up a Sensate Focus video room. Present a pre-recorded, accessible, and easy-to-understand video on Sensate Focus techniques25,26.
- Set up a simulated family room. Use this space to demonstrate Sensate Focus techniques to patients and their partners.
- Set up a testing room to conduct audiovisual sexual stimulation (AVSS) and penile erection rigidity testing. These tests help exclude organic causes of ED or meet patient requests for further evaluation27.
3. Implementation of the GLTC framework
- Integrate the three elements of effective doctor-patient communication-Goodwill (G), Listening (L), and Talking (T)-into the consultation process to focus on the patient's needs, emotions, and expectations. This approach fosters a patient-centered method that enhances the doctor-patient relationship and ultimately leads to Cooperation (C), forming a closed-loop communication model.
- Apply the GLTC framework to the case of a couple seeking consultation due to unconsummated marriage (UCM), as described in the following example:
- Goodwill (G)
- Be kind and friendly to patients. Provide a quiet room with appropriate decor that ensures privacy, allowing them to communicate in a comfortable and relaxed setting.
- Listening (L)
- Give the patient ample time to express their doubts and concerns. Avoid interrupting the patient, but respond appropriately when necessary.
- Carefully listen and identify the patient's needs and expectations.
- Talking (T)
- Patiently and clearly answer the patient's questions, building upon active listening and an understanding of the patient's emotional responses.
- Address the patient's emotional and psychological needs while actively responding to their expectations to establish the foundation for cooperation.
- Cooperation (C)
- Promote consensus between the patient and their partner and establish a cooperative doctor-patient relationship to jointly address the medical, psychological, and social challenges associated with UCM.
- Goodwill (G)
4. Treatment procedure
- Initial consultation
- Ensure that physicians review the patient's preliminary information and conduct a comprehensive interview using GLTC communication techniques to foster a relaxed and trusting atmosphere.
- Identify psychological factors using the Hawton classification15 to develop a personalized treatment plan (see Figure 1C).
- Physical examination and testing
- Perform a physical examination of the patient.
- Conduct additional laboratory tests, such as fasting blood glucose, lipid profile, and testosterone levels. Perform penile rigidity assessments, including audiovisual sexual stimulation (AVSS) or penile erection rigidity testing, if necessary.
- Sexual and psychological education
- Ensure that the nurse provides 15-20 min of education to the patient and their partner, addressing questions and maintaining a supportive environment using the GLTC framework.
- Self-study on sexual health
- Ensure that the patient and their partner spend 20-30 min in the self-study room reviewing educational materials or videos based on the issues identified during earlier sessions.
- Sensate Focus Demonstration under medical staff guidance
- Ensure that the couple watches a 50-min Sensate Focus demonstration video to learn cognitive-behavioral sexual therapy techniques.
NOTE: Steps 4.3-4.5 can be adjusted based on patient scheduling and progress; however, all must be completed before proceeding to step 4.6.
- Ensure that the couple watches a 50-min Sensate Focus demonstration video to learn cognitive-behavioral sexual therapy techniques.
- Practicing Sensate Focus in the simulated family room
- Ensure that the couple practices key Sensate Focus steps under nurse guidance while clothed.
- Ensure that the nurse explains concepts and guides them through the three stages: Non-genital Touching, Genital and/or Breast Touching, and Sensual Intercourse.
- Ensure a gynecological examination is conducted for the partner, if necessary, to rule out any contributing female factors.
- Instruct the couple to continue practicing these steps at home.
- Follow-up and adjustment
- Schedule an 8-week follow-up visit during the Sensual Intercourse stage to assess outcomes such as sexual performance and anxiety levels (using the IIEF-5 questionnaire), and frequency of intercourse and to guide further treatment.
- Encourage the couple to engage in sexual intercourse at least once per week.
- Prescribe phosphodiesterase-5 (PDE5) inhibitors (sildenafil citrate tablets) to support the sensual intercourse stage if the patient demonstrates low confidence.
5. Data collection
- Collect demographic data from the hospital information system.
- Record the frequency of masturbation based on relevant literature(28) to explore its potential association with psychogenic erectile dysfunction (pED), which informs targeted sex education and behavioral therapy.
NOTE: Light masturbation is defined as an average of one masturbation episode every 4 days or more; Frequent masturbation is defined as an average of one masturbation episode every 3 days or less; Excessive masturbation is defined as frequent masturbation persisting for more than 2 years. - Measure the following scores:
- International Index of Erectile Function (IIEF-5) score (range: 5-25)23, used to evaluate erectile function and classify severity as: Severe (5-7), Moderate (8-11), Mild-to-moderate (12-16), Mild (17-21), Normal (22-25). This provides a standardized assessment of treatment efficacy.
- Erection Hardness Score (EHS) (range: 0-4)29: 0 - Penis does not enlarge, 1 - Enlarged but not hard, 2 - Hard but not hard enough for penetration, 3 - Hard enough for penetration but not completely hard, 4 - Fully rigid and hard. This offers a simple evaluation of erectile quality.
- The number of patients responding "yes" to Sexual Encounter Profile questions: SEP-Q2: Was the erection hard enough for penetration? SEP-Q3: Was the erection maintained long enough for successful intercourse?30,31.
- Sexual Satisfaction Score for Women (SSS-W) (scale: 1-5)32: 1 - Very dissatisfied, 2 - Dissatisfied, 3 - Neutral, 4 - Satisfied, 5 - Very satisfied. This provides a straightforward assessment of the female partner's sexual satisfaction.
- Record the number of patients who received phosphodiesterase-5 (PDE5) inhibitors (sildenafil citrate tablets).
- Track the number of female partners who achieved pregnancy during the follow-up period.
6. Validation of protocol and evaluation of treatment efficacy
- Follow standard principles for taking a sexual history and differentiate between primarily psychological and primarily organic erectile dysfunction (ED), in conjunction with self-rating scale results (Supplementary File 1, Supplementary Tables 1, and Supplementary Table 2).
- Identify and document psychological factors contributing to ED using the Hawton classification15 (Supplementary File 1, and Supplementary Table 3).
- Clearly explain the treatment process and specific procedural steps to the patient and their partner, and obtain informed consent.
- Complete at least the first six steps of the protocol (steps 4.1-4.6) once every 2 weeks over a duration of 8 weeks, constituting one full treatment course.
- Evaluate treatment efficacy following one course using the following criteria:
- An increase of three or more points in the patient's International Index of Erectile Function (IIEF-5) score compared to baseline.
- An Erection Hardness Score (EHS) of ≥3 for the patient and a Sexual Satisfaction Score for Women (SSS-W) of ≥3 for the partner.
- A proportion of "Yes" responses exceeding 80% for both Sexual Encounter Profile questions SEP-Q2 (erection sufficient for penetration) and SEP-Q3 (erection maintained for completion of intercourse) (Supplementary File 1, Supplementary Table 1, Supplementary Table 4, Supplementary Table 5, and Supplementary Table 6).
Wyniki
A total of 64 patients and their partners were admitted to the study. Of these, 22 couples (32.2%) discontinued treatment after the initial assessment. The primary reasons for treatment interruption were time constraints affecting both partners, difficulties related to travel distance, and preference for alternative therapies such as traditional Chinese medicine. Additional contributing factors may have included psychological barriers, such as embarrassment or stigma, lack of immediate treatment effects, and insufficient support systems. The remaining 42 couples (67.8%) completed the full treatment protocol and were followed up to the 16th week. These couples reported a successful intercourse rate -- defined as achieving vaginal penetration and completing sexual intercourse during the treatment period -- of over 80% (30/36), based on self-reported follow-up data. Two patients were referred for individualized psychological counseling. Six couples did not complete the follow-up assessments.
The mean age of the 42 male patients was 28.9 ± 5.4 years, and the duration of unconsummated marriage (UCM) ranged from 3 months to 2.5 years. To better understand the demographic characteristics of the patient population, factors such as educational background, regional economic status, and masturbation habits were analyzed in comparison with historical data from similar cases in the region. Among the 42 patients, 28.6% (12/42) had a college degree or higher, while 71.4% (30/42) had a secondary education or lower. Most patients (78.6%, 33/42) came from economically developing areas. A history of masturbation was reported by 88% (37/42) of patients. Of these, 37.8% (14/37) engaged in light masturbation, and 62.2% (23/37) in frequent masturbation. Among those with frequent masturbation, 60.1% (14/23) were classified as excessive masturbators, often linked to a lack of sexual knowledge. The development of masturbation habits was attributed to several factors. Nearly half (45.9%, 17/37) began masturbating after frequently touching their external genitalia. Other influences included exposure to online or other sexually explicit videos, and peer suggestions to try masturbation, which eventually formed into a habitual behavior. Post-marriage or cohabitation, the masturbation rate was 32.4% (12/37).
Psychological analysis using the Hawton classification15 indicated that lack of sex education and sexual trauma associated with masturbation was common predisposing factors for primary erectile dysfunction (pED). Additionally, 69% (29/42) of patients reported experiencing sexual anxiety. Avoidance of sexual activity and infertility-related pressure were key precipitating factors, while poor communication -- often due to a dominant female partner -- was a frequent maintenance factor. High masturbation frequency was found to correlate with lower education levels and the underdeveloped economic background of the patients' upbringing. These findings align with the Hawton classification, highlighting inadequate sex education as a shared feature among the patients. During initial interviews, 50% (21/42) of the men appeared passive, often seeking consultation due to pressure from their partner or family rather than personal motivation.
Significant improvements were observed across key assessment parameters, including the International Index of Erectile Function-5 (IIEF-5), Erection Hardness Score (EHS), and Sexual Satisfaction Scale for Women (SSS-W). The mean IIEF-5 score increased markedly from 5.1 ± 1.1 at baseline to 18.9 ± 2.8 post-treatment, with a slight decrease to 17.6 ± 2.7 at the 8-week follow-up, indicating sustained treatment efficacy. Similarly, the mean EHS score improved from 1.5 ± 0.7 at baseline to 3.6 ± 0.5 post-treatment, with a slight reduction to 3.5 ± 0.5 at 8 weeks. The mean SSS-W score, reflecting female partner sexual satisfaction, increased from 1.3 ± 0.5 at baseline to 3.8 ± 0.6 post-treatment and further to 3.9 ± 0.6 at follow-up. All improvements were statistically significant both immediately post-treatment and at the 8-week follow-up (p < 0.05), suggesting durable therapeutic effects. Evaluation using the Sexual Encounter Profile (SEP) questions showed notable improvements. The rate of successful penile penetration (SEP-Q2) rose significantly from 19% pre-treatment to 83.3% post-treatment, and remained high at 75.0% at the 8-week follow-up (p < 0.01). The success rate of completed sexual intercourse (SEP-Q3) increased from 0% at baseline to 81.0% post-treatment, and further to 83.3% at follow-up (p < 0.01), as shown in Table 1. Among the 42 couples, 31% (13/42) of patients required the use of PDE5 inhibitors (sildenafil citrate tablets, Pfizer Inc.) to complete the sensual intercourse stage. Notably, 11 female partners reported successful pregnancies during the 8-month follow-up period.
A representative case involved a 28-year-old male who reported poor erectile function over the past year following marriage. The patient had a history of excessive masturbation beginning at age 13. He married in 2020, and the couple attempted intercourse 4-6 times within the first three months, all of which were unsuccessful, leading to unconsummated marriage (UCM). The patient described an initial erectile response that diminished rapidly within 3-5 min during foreplay. Erections became insufficient for penetration, leading to heightened anxiety around sexual activity. Despite being married, he continued to masturbate and reported a low sexual drive, attempting intercourse only 2-3 times per month, all unsuccessful. He also avoided sexual activity entirely due to performance anxiety. Infertility emerged as the most pressing consequence of UCM, prompting the couple to seek medical assistance under family pressure. After evaluation, the patient met the study inclusion criteria. Organic erectile dysfunction was excluded through normal blood glucose, lipid profile, and penile rigidity assessments.
Through a comprehensive assessment of the patient's medical history and the application of Hawton's classification of psychological factors, sexual trauma resulting from inadequate sexual education and a history of excessive masturbation were identified as predisposing factors contributing to psychogenic erectile dysfunction (pED). These factors were systematically evaluated using the checklist of psychological factors associated with ED (Supplementary Table 3), which categorizes psychological influences into predisposing, precipitating, and maintaining factors, ensuring a structured and thorough diagnostic approach. In addition, the patient exhibited sexual anxiety and avoidance of sexual activity, which, combined with familial pressure related to infertility, acted as precipitating and maintaining factors in the development and persistence of pED.
Following a detailed consultation and the use of GLTC communication techniques, a personalized treatment plan was formulated. This plan integrated targeted education on sexual and psychological health, emphasizing sexual function, partner communication, and stress management strategies. The plan also incorporated Sensate Focus therapy. During therapy, the patient experienced insufficient penile rigidity during the third stage of Sensate Focus. To address this, the clinician prescribed a PDE5 inhibitor (50 mg sildenafil citrate tablet) to be taken 1 h before sexual activity. The patient successfully completed the entire treatment course. Over time, improvements in self-confidence (as assessed by Question 1 of the IIEF-5) and marital satisfaction (Question 5 of the IIEF-5) (Supplementary Table 1) were recorded using standardized questionnaires and self-reports. The patient's progress culminated in a successful pregnancy of the partner during the follow-up period.
DATA AVAILABILITY:
Provided in Supplementary File 1.
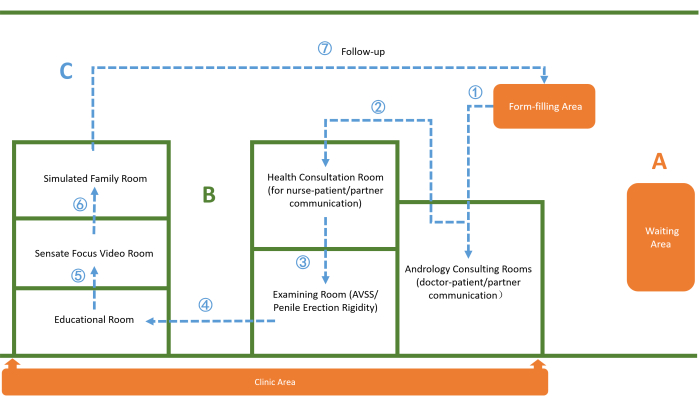
Figure 1: Layout of rooms and patient movement flow in the andrology area. (A) Andrology Area Layout (Orange): Comprises the waiting area, form-filling area, and clinic area. (B) Room Layout (Green): Depicts seven independent rooms designated for consultation, therapy, and examination. (C) Patient Movement Flow (Blue): Illustrates the treatment process from registration through follow-up. Please click here to view a larger version of this figure.
| Assessed parameters | Before therapy | After treatment | N | P* | 8 weeks of follow-up after treatment | N | P** |
| IIEF-5 | 5.1 ± 1.1 | 18.9 ± 2.8 | 42 | 0.000 | 17.6 ± 2.7 | 36 | 0.000 |
| EHS | 1.5 ± 0.7 | 3.6 ± 0.5 | 42 | 0.000 | 3.5 ± 0.5 | 36 | 0.000 |
| SEP-Q2 | 8 (19.0%) | 35 (83.3%) | 42 | 0.000 | 27 (75.0%) | 36 | 0.000 |
| SEP-Q3 | 0 (0%) | 34 (81.0%) | 42 | 0.000 | 30 (83.3%) | 36 | 0.000 |
| SSS-W | 1.3±0.5 | 3.8±0.6 | 42 | 0.000 | 3.9±0.6 | 36 | 0.000 |
Table 1: Summary of assessed parameters across different treatment stages. Data are presented as mean ± standard deviation (SD). *Indicates a comparison between baseline and post-treatment values. ** Indicates a comparison between baseline and 8-week follow-up values. Abbreviations: IIEF-5 - International Index of Erectile Function-5, EHS - Erection Hardness Score, SEP-Q2 - Sexual Encounter Profile Question 2 (adequate erection for penetration), SEP Q3 - Sexual Encounter Profile Question 3 (erection maintenance until completion), SSS-W - Sexual Satisfaction Score for Women.
Supplementary Table 1: The International Index of Erectile Function-5 (IIEF-5) questionnaire. Please click here to download this File.
Supplementary Table 2: Characteristics used to distinguish psychogenic from organic sexual dysfunction. Please click here to download this File.
Supplementary Table 3: Checklist of psychological factors associated with erectile dysfunction. Please click here to download this File.
Supplementary Table 4: The Erection Hardness Score (EHS). Please click here to download this File.
Supplementary Table 5: The Sexual Satisfaction Scale for Women (SSS-W). Please click here to download this File.
Supplementary Table 6: Sexual Encounter Profile (SEP) questions. Please click here to download this File.
Supplementary File 1: Raw dataset used in the analysis. Please click here to download this File.
Dyskusje
In cases of unexplained couple mismatch (UCM), primary erectile dysfunction (pED) is recognized as the predominant etiology in males. It is characterized by cognitive-behavioral constructs such as performance anxiety, self-efficacy deficits, and sexual avoidance patterns, as delineated in Hawton's psychosexual triaxial classification33,34. Current evidence indicates that monotherapy approaches exhibit limited long-term efficacy35. Contemporary guidelines propose algorithm-driven protocols for the management of patients with erectile dysfunction (ED)36,37; however, this does not equate to a comprehensive service system for ED within andrology specialties38, which often lack multidisciplinary team efforts39, particularly in developing regions40. The credentialing of sex therapists and the establishment of psychosexual therapy teams remain challenging in these areas. Meanwhile, the impact of UCM on couples cannot be overlooked. If psychological factors are present in males with ED, these should at least be acknowledged and appropriately treated. An integrative approach -- combining both medical and therapeutic models -- is proposed, utilizing a streamlined management framework with phases ranging from assessment to intervention when addressing such patients.
To address these clinical challenges, systematic training programs were implemented for medical staff to enhance competencies in sexual medicine and cognitive-behavioral frameworks. Hawton's triaxial psychosexual classification proved instrumental in psychological profiling. Concurrently, healthcare teams completed GLTC (Goodwill-Listening-Talking-Cooperation) communication training, operationalized through four sequential pillars: establishing therapeutic rapport, empathetic inquiry, collaborative goal-setting, and partnership reinforcement. This patient-centric framework -- distinct from the Liverpool Communication Skills Assessment Scale (LCSAS)41 and the professional-dependent protocols of Cognitive Behavioral Therapy (CBT)42 -- enables efficient identification of ED-related psychosocial determinants (e.g., sexual literacy deficits) through structured dialogue, circumventing the need for resource-intensive psychotherapy. Furthermore, institutional collaborations with regional health administrations have led to the establishment of novel billing codes for time-intensive psychosexual education, including reality-based scenario simulations, to optimize counseling efficiency within constrained clinical workflows.
With these foundational efforts, a protocol suitable for simple andrology teams to treat primary erectile dysfunction (pED) and guide UCM couples toward successful intercourse has been developed. Key innovations focus on a patient-centered approach through the GLTC communication framework, emphasizing tailored strategies -- including active listening, psychological stage identification, empathetic communication, and simplified educational tools -- to improve trust, reduce anxiety, and rebuild confidence. This approach has proven particularly effective in addressing psychogenic sexual dysfunction.
The protocol emphasizes comprehensive psychosexual evaluation using Hawton's triaxial classification model to identify key pED determinants, including sexual literacy deficits, compulsive masturbatory patterns, and performance anxiety neuroses. Central to this framework is the GLTC (Goodwill-Listening-Talking-Cooperation) communication paradigm, which fosters therapeutic alliances by aligning clinician responses with patients' psychological trajectories -- typically progressing through phases of shock-denial, guilt-anger, and depression. Notably, 32.73% of outpatient dissatisfaction stems from communication failures, often due to clinicians' inability to manage countertransference reactions during emotionally charged interactions. The GLTC model addresses this through phase-specific empathetic engagement: identifying psychological transition nodes, deploying pED-targeted psychoeducation, and cultivating adaptive cognitive reframing.
Simultaneously, care delivery transitions from a disease-centric to a family-inclusive model, operationalized via an integrated, streamlined multi-room system accommodating both physiological and psychological aspects. This model addresses biomedical, relational, and reproductive dimensions through coordinated cross-disciplinary workflows. The duration of UCM treatment typically spans six months. However, clinical observations suggest that the longer treatment continues -- especially beyond three months without successful intercourse -- the more difficult subsequent interventions become, with outcomes such as divorce becoming more likely43. While pED leading to UCM can be treated through non-drug methods such as psychotherapy44, these approaches show only moderate success, often requiring prolonged treatment and demonstrating high recurrence rates. As such, they may be unsuitable for patients under reproductive pressure after marriage, particularly since most couples with UCM present with the primary intent to conceive rather than to consummate the marriage. Studies have shown that if these issues are not effectively resolved, some couples eventually divorce, with 75% of such cases occurring within six months of UCM onset45,46.
According to previous studies47,48, oral medications such as sildenafil and tadalafil have brought about a pharmaceutical and biotechnological revolution in UCM treatment, with success rates of up to 100% and 91%, respectively. Therefore, adjustments are made during the third phase of Sensate Focus49. If confidence or erectile response remains insufficient, patients are counseled about and prescribed a PDE5 inhibitor to ensure success within three months. With a well-structured and streamlined management strategy guided by the philosophy of the integrative approach, this method does not significantly increase the psychological burden. Importantly, the success of penovaginal penetration is not the sole goal of the treatment model. The broader objective is to assess the medium- and long-term satisfaction of couples following consummation. Even after discontinuation of medication, patients may choose to use PDE5 inhibitors independently and continue to prioritize mutual support and communication, thereby maintaining high levels of satisfaction.
However, challenges remain, including the time-intensive nature of the diagnostic and treatment processes, which require sustained patience and enthusiasm from healthcare providers, as well as the necessity for ongoing education in sexual medicine, psychology, and patient care. There are several limitations to this study. The findings are preliminary, and the current research primarily involves patients from a single geographic region, which may limit the generalizability of the results. Additionally, the sample size is relatively small. To validate these findings and enhance their generalizability, future studies should include larger-scale, multi-center investigations involving diverse patient populations from various regions. This would help ensure that the model is applicable across different demographic and cultural backgrounds.
This approach focused particularly on cases primarily involving male factors, with erectile dysfunction (ED) resulting from unexplained couple mismatch (UCM). Some partners of UCM patients became pregnant. Although the follow-up duration was not sufficient, tracking pregnancy outcomes remains vital in evaluating the success of this treatment model, as it directly addresses the ultimate goal of resolving infertility associated with pED in UCM cases. While improvements in erectile function, psychological well-being, and partner satisfaction are important indicators of treatment efficacy, the ability to achieve a successful pregnancy demonstrates the model's impact on overcoming reproductive challenges. Monitoring pregnancy outcomes allows clinicians to assess the effectiveness of the integrative approach in restoring sexual function, fostering emotional and relational stability, and enabling couples to conceive naturally.
The study currently focuses on evaluating the preliminary effects of the intervention within a limited timeframe, which is nevertheless crucial and highly relevant to clinical practice. Moreover, the goal is for patients to achieve vaginal intercourse within 16 weeks; failure to meet this objective may significantly increase the difficulty of treatment for both partners. These 8-week intervals are considered integral components of the therapy. Unlike traditional pharmacological treatments, this process requires healthcare professionals to engage in attentive listening and responsive communication, ensuring that patients gradually overcome psychological barriers identified through screening based on Hawton's classification model. This approach helps alleviate anxiety, enhances understanding, and promotes better communication between partners, underscoring the importance and significance of the model.
Of course, the GLTC framework has its limitations. As a communication tool, it cannot fully substitute for cognitive behavioral therapy (CBT) or formal psychotherapy. In instances where the GLTC model fails to adequately resolve psychological issues -- for example, two couples in this study with significant psychological symptoms or relational conflicts remained unresponsive -- referral to a specialized, comprehensive sexual medicine team was necessary.
The dropout of 22 patients is notable, and efforts are ongoing to understand the underlying reasons. In this study, three main contributors to treatment discontinuation were identified: scheduling difficulties for both partners, inconvenience caused by travel distance, and preference for alternative therapies such as traditional Chinese medicine. Further research is needed to explore how a strategically integrated multidisciplinary approach can be implemented earlier in the course of treatment. Early intervention may increase the chances of preserving the relationship, particularly when considering both the sexual satisfaction and procreative goals of the couples.
Overall, this treatment model presents a practical, scalable, and effective solution grounded in current treatment guidelines for ED. It addresses not only the needs of basic andrology teams but also the diverse clinical demands of patients with ED and related conditions such as dyspareunia, lack of sexual knowledge, and unsuccessful intercourse due to premature ejaculation.
Ujawnienia
The authors have no conflicts of interest to disclose.
Podziękowania
This work was supported by a grant from the Research Project of Teaching Reform in Clinical Teaching Base of General Medical Colleges in Guangdong Province, DEPARTMENT OF EDUCATION OF GUANGDONG PROVINCE, with Grant Number of 2023-32-190, Fundamental Research Funds for the Central Universities, Sun Yat-sen University, with Grant Number of 2024008, and Teaching Improvement Plan of 2023 of the Affiliated Panyu Central Hospital, Guangzhou Medical University.
Materiały
| Name | Company | Catalog Number | Comments |
| Anatomical Illustrations of the Male and Female Reproductive Systems | Rui'an Shengxiao Plastic Products, China | L08 | llustrations for educational purposes. |
| Anatomical Model of Female Reproductive System | Rui'an Shengxiao Plastic Products, China | A200 | Detailed anatomical model for educational purposes. |
| Anatomical Model of Male Reproductive System | Rui'an Shengxiao Plastic Products, China | A100 | Detailed anatomical model for educational purposes. |
| Andrology Consulting Rooms | N/A | N/A | Two dedicated andrology consulting rooms designed for comprehensive doctor-patient and partner communication. See Figure 1B. |
| Andrology Consulting Rooms | N/A | N/A | Used for doctor-patient/partner communication, each doctor trained in GLTC communication skills. |
| Audiovisual Sexual Stimulation (AVSS) / Penile Erection Rigidity Testing Room | N/A | N/A | This specialized room is equipped for audiovisual sexual stimulation (AVSS) and penile erection rigidity testing. It provides a controlled environment for evaluating erectile function. See Figure 1B. |
| Checklist of Psychological factors associated with erectile dysfunction Modified from Hawton classification, conducted in interview. | N/A | N/A | Supplemental Table S3. |
| Clinic Area | N/A | N/A | This are is the core of the clinic, featuring multiple consultation and examination rooms for various diagnostic and treatment activities. The layout with seven independent Rooms is carefully designed to ensure efficient workflows and privacy. See Figure 1A. |
| Data collecting table | N/A | N/A | The header columns in the table display the necessary information or evaluation criteria to be collected during the diagnosis and treatment process.See Data available.xls. |
| Doctor-Patient Communication (2nd Edition) | People's Medical Publishing House, China | ISBN 978-7-117-26404-4 | GLTC communication skills Training Materials. |
| Educational Room | N/A | N/A | Educational room is a resource-rich environment, stocked with a variety of health education materials designed to cater to the diverse needs of our patients sexual and psychological health. It features anatomical models of male and female reproductive organs and penis erection hardness models and includes educational Videos. Educational Videos provide visual and auditory learning experiences, making complex medical concepts more accessible. These videos cover a range of topics, including preventive health measures, treatment options, and lifestyle modifications. This room serves as an educational hub, allowing patients and their partners to gain a deeper understanding of reproductive health through hands-on learning and reading materials. See Figure 1B. |
| Form of characteristics for distinguishing psychologic from organic sexual dysfunction, conducted in interview. | N/A | N/A | Supplemental Table S2. |
| Form of the Erection Hardness Score (EHS) | N/A | N/A | Supplemental Table S4. |
| Form-Filling Area | N/A | N/A | Equipped with desks, chairs, pens, and all required forms and materials to ensure that patients can easily complete their necessary medical information and questionnaires. Electronic form can be another option. See Figure 1A. |
| Functional zoning of the Andrology Clinic area | N/A | N/A | Including Waiting Area, Form-Filling Area and Clinic Area. This functional zoning not only maximizes the use of limited space but also ensures a rational and efficient diagnostic process. Through scientific layout and zoning, we can provide a better service experience for patients while improving the quality and efficiency of our medical services. See Figure 1A. |
| Health Consultation Room | N/A | N/A | Used for nurse-patient/partner communication, each nurse trained in GLTC communication skills, ensuring that patients receive well-rounded care and support. See Figure 1B. |
| Layout of the seven independent Rooms | N/A | N/A | The clinic area recommended comprises seven independent rooms, each tailored to specific aspects of patient care and education. See Figure 1B-1C. |
| Penis Erection Hardness Models | Pfizer Inc. | EHM-001 | The Erection Hardness Model by Pfizer Inc. is a comprehensive educational tool designed to help healthcare professionals assess and discuss erectile function with patients. The model illustrates various levels of erection hardness, providing a clear and practical reference for both diagnosis and patient education. This tool aids in improving communication and understanding between doctors and patients regarding erectile health. |
| RigiScan | Gotop Medica, US | Plus | RigiScan Plus is a product of Gesiva Medical, which specializes in medical devices for diagnosing and assessing erectile dysfunction. |
| Sensate Focus video | MFP Power Supply Company | Sensate Focus video room featuring videos from the “SEX, A Life Long Pleasure”, produced by MFP Power Supply Company, presented by Belgian and American sexologists and psychologists. | |
| Sensate Focus Video Room | N/A | N/A | This room is dedicated to Sensate Focus training, featuring instructional videos from the series "SEX, A Life Long Pleasure," produced by MFP Power Supply Company. The videos are presented by renowned Belgian and American sexologists and psychologists, providing patients and their partners with expert guidance on maintaining a healthy sexual life. See Figure 1B. |
| Sexual Encounter Profile (SEP) questions 2, 3 | N/A | N/A | Supplemental Table S6. |
| Sildenafil citrate tablet | Pfizer Inc. | Film coated, 5x100mg/capsule | For patients with Erectile Dysfunction when necessary. |
| Simulated Family Room | N/A | N/A | The simulated family room is used exclusively to demonstrate to patients and their partners with normal dresses how to practice each step of Sensate Focus at home. This realistic setting helps couples learn and rehearse the techniques in a familiar environment, enhancing the effectiveness of their home practice. See Figure 1B. |
| The International Index of Erectile Function 5 (IIEF-5) questionnaire | N/A | N/A | Table S1. |
| The Sexual Satisfaction Scale for Women (SSS-W) | N/A | N/A | Supplemental Table S5. |
| Waiting Area | N/A | N/A | Equipped with comfortable seating, reading materials, and health education videos to help patients understand more about their health and the diagnostic process during their wait. See Figure 1A. |
Odniesienia
- Mccabe, M. P., et al. Definitions of sexual dysfunctions in women and men: A consensus statement from the fourth international consultation on sexual medicine 2015. J Sex Med. 13 (2), 135-143 (2016).
- Aydin, S., et al. Multicentral clinical evaluation of the aetiology of erectile dysfunction: A survey report. Int Urol Nephrol. 32 (4), 699-703 (2001).
- Sánchez De La Vega, J., Amaya Gutiérrez, J., Alonso Flores, J. J., García Pérez, M. erectile dysfunction in those under 40. Etiological and contributing factors. Arch Esp Urol. 56 (2), 161-164 (2003).
- Krishnappa, P., et al. Unconsummated marriage: A systematic review of etiological factors and clinical management. J Sex Med. 21 (1), 20-28 (2023).
- Shamloul, R. Management of honeymoon impotence. J Sex Med. 3 (2), 361-366 (2006).
- Badran, W., et al. Etiological factors of unconsummated marriage. Int J Impot Res. 18 (5), 458-463 (2006).
- Ozdemir, O., Simsek, F., Ozkardeş, S., Incesu, C., Karakoç, B. The unconsummated marriage: Its frequency and clinical characteristics in a sexual dysfunction clinic. J Sex Marital Ther. 34 (3), 268-279 (2008).
- Mims-Gillum, P. 114 I do....Not! Consummating the unconsummated marriage. J Sex Med. 16 (Supplement_3), S44-S44 (2019).
- Dewitte, M., et al. A psychosocial approach to erectile dysfunction: Position statements from the European Society of Sexual Medicine (ESSM). Sex Med. 9 (6), 100434(2021).
- Grover, S., Shouan, A. Assessment scales for sexual disorders-a review. J Psychosex Health. 2 (2), 121-138 (2020).
- Schmidt, H. M., Munder, T., Gerger, H., Frühauf, S., Barth, J. Combination of psychological intervention and phosphodiesterase-5 inhibitors for erectile dysfunction: A narrative review and meta-analysis. J Sex Med. 11 (6), 1376-1391 (2014).
- Simopoulos, E. F., Trinidad, A. C. Male erectile dysfunction: Integrating psychopharmacology and psychotherapy. Gen Hosp Psychiatry. 35 (1), 33-38 (2013).
- Koon, C. S., et al. The phosphodiasterase 5-inhibitors (pde-5i) for erectile dysfunction (ed): A therapeutic challenge for psychiatrists. Curr Drug Targets. 19 (12), 1366-1377 (2018).
- Hawton, K., Catalan, J. Prognostic factors in sex therapy. Behav Res Ther. 24 (4), 377-385 (1986).
- Avasthi, A., Grover, S., Sathyanarayana Rao, T. S. Clinical practice guidelines for management of sexual dysfunction. Indian J Psychiatry. 59 (Suppl 1), S91-S115 (2017).
- Althof, S. E., Needle, R. B. Psychological and interpersonal dimensions of sexual function and dysfunction in women: An update. Arab J Urol. 11 (3), 299-304 (2013).
- Jianwen, S., Qun, L., Jinfan, W. Analysis and effect evaluation of the intervention using GLTC doctor-patient communication program for inpatients. Chin J Hosp Admin. 36 (11), 5(2020).
- Shao Jianwen, T. G., et al. A comparative study on the influence of outpatient experience communication and GLTC communication on doctors' emotional state and communication details of outpatient doctors. Chin Gen Prac. 27 (16), 6(2024).
- Jinfan, S. J. L. Q. W. Analysis and effect evaluation of the intervention using GLTC doctor-patient communication program for inpatients. Chin J Hosp Manag. 36 (11), 5(2020).
- Fei Yan, J. W. Construction of an educational model guided by the "GLTC" doctor-patient communication model. Guide Sci Ed-Electon Ed. 0000 (012), 2(2021).
- Ha, J. F., Longnecker, N. Doctor-patient communication: A review. Ochsner J. 10 (1), 38-43 (2010).
- Kaminsky, A., Sperling, H., Popken, G. Primary and secondary prevention of erectile dysfunction. Urologe A. 50 (10), 1265-1268 (2011).
- Rosen, R. C., Cappelleri, J. C., Gendrano, N. The international index of erectile function (IIEF): A state-of-the-science review. Int J Impot Res. 14 (4), 226-244 (2002).
- Symonds, T., Perelman, M. A., Althof, S., et al. Development and validation of a premature ejaculation diagnostic tool. Eur Urol. 52 (2), 565-573 (2007).
- Masters, W. H., Johnson, V. E. Human sexual inadequacy. , (1970).
- Mccabe, M. P., Althof, S. E. Issm guidelines for the diagnosis and treatment of erectile dysfunction. J Sex Med. 20, 1-20 (2023).
- Wang, T., et al. Audiovisual sexual stimulation and rigiscan test for the diagnosis of erectile dysfunction. Chin Med J (Engl). 131 (12), 1465-1471 (2018).
- Huang, S., Nyman, T. J., Jern, P., Santtila, P. Actual and desired masturbation frequency, sexual distress, and their correlates. Arch Sex Behav. 52 (7), 3155-3170 (2023).
- Goldstein, I., et al. The erection hardness score and its relationship to successful sexual intercourse. J Sex Med. 5 (10), 2374-2380 (2008).
- Shabsigh, R., et al. Reliability of efficacy in men with erectile dysfunction treated with tadalafil once daily after initial success. Int J Impot Res. 22 (1), 1-8 (2010).
- Belkoff, L. H., et al. An open-label, long-term evaluation of the safety, efficacy and tolerability of avanafil in male patients with mild to severe erectile dysfunction. Int J Clin Pract. 67 (4), 333-341 (2013).
- Lee, J. T., Hu, Y. L., Meston, C. M., Lin, H. H., Tseng, H. M. The sexual satisfaction scale for women (SSS-W): Adaptation and validation of a traditional Chinese version in Taiwan. J Sex Marital Ther. 45 (3), 179-189 (2019).
- Xi, Y., et al. Unconsummated marriage among Chinese couples: A retrospective study. Sex Med. 11 (1), qfac003(2023).
- Murugan, S. Unconsummation of marriage. J Psychosex Health. 3 (3), 283-285 (2021).
- Caskurlu, T., Tasci, A. I., Resim, S., Sahinkanat, T., Ergenekon, E. The etiology of erectile dysfunction and contributing factors in different age groups in Turkey. Int J Urol. 11 (7), 525-529 (2004).
- Hackett, G., et al. British Society for sexual medicine guidelines on the management of erectile dysfunction in men-2017. J Sex Med. 15 (4), 430-457 (2018).
- Burnett, A. L., et al. Erectile dysfunction: Aua guideline. J Urol. 200 (3), 633-641 (2018).
- Giacomo Ciaccio, V., Di Giacomo, D. Psychological factors related to impotence as a sexual dysfunction in young men: A literature scan for noteworthy research frameworks. Clin Pract. 12 (4), 501-512 (2022).
- Hao, S. W. Sex therapy is effective for erectile dysfunction. Zhonghua Nan Ke Xue. 14 (6), 538-541 (2008).
- Salonia, A., et al. European Association of Urology guidelines on sexual and reproductive health-2021 update: Male sexual dysfunction. Eur Urol. 80 (3), 333-357 (2021).
- Qureshi, A. A., Zehra, T. Simulated patient's feedback to improve communication skills of clerkship students. BMC Med Educ. 20 (1), 15(2020).
- Lewis, R. W., et al. Epidemiology/risk factors of sexual dysfunction. J Sex Med. 1 (1), 35-39 (2004).
- Naseri, A., et al. Unconsummated marriage. Health. 7 (7), 3(2015).
- Brotto, L., et al. Psychological and interpersonal dimensions of sexual function and dysfunction. J Sex Med. 13 (4), 538-571 (2016).
- Banerjee, K., Singla, B. Pregnancy outcome of home intravaginal insemination in couples with unconsummated marriage. J Hum Reprod Sci. 10 (4), 293-296 (2017).
- Zargooshi, J. Unconsummated marriage: Clarification of aetiology; treatment with intracorporeal injection. BJU Int. 86 (1), 75-79 (2000).
- Perelman, M. A. Fsd partner issues: Expanding sex therapy with sildenafil. J Sex Marital Ther. 28 (Suppl 1), 195-204 (2002).
- Ghanem, H., El-Dakhly, M., Shamloul, R. Alternate-day tadalafil in the management of honeymoon impotence. J Sex Med. 5 (6), 1451-1454 (2008).
- Atallah, S., Haydar, A., Jabbour, T., Kfoury, P., Sader, G. The effectiveness of psychological interventions alone, or in combination with phosphodiesterase-5 inhibitors, for the treatment of erectile dysfunction: A systematic review. Arab J Urol. 19 (3), 310-322 (2021).
Przedruki i uprawnienia
Zapytaj o uprawnienia na użycie tekstu lub obrazów z tego artykułu JoVE
Zapytaj o uprawnieniaThis article has been published
Video Coming Soon
Copyright © 2025 MyJoVE Corporation. Wszelkie prawa zastrzeżone