Method Article
Improved Home Blood Pressure Control by CT-guided Ozone-mediated Renal Denervation for Patients with Resistant Hypertension
* These authors contributed equally
In This Article
Summary
CT-guided ozone-mediated renal denervation (RDN) by injecting an O2-O3 gas mixture around lumbar ganglia reduces antihypertensive medication burden and achieves an improved home blood pressure control rate. We present a novel, simplified, unilateral, and contrast-free RDN technique that minimizes the renal artery injury in the treatment of patients with resistant hypertension (RH).
Abstract
Accumulating evidence from clinical trials in recent years has consistently supported the blood pressure (BP)-lowering efficacy of renal sympathetic denervation (RDN). However, the most widely used catheter-based RDN technique still has limitations in clinical practice. Therefore, it is necessary to develop an alternative RDN approach for BP control. In our previous clinical trial, we demonstrated that CT-guided ozone-mediated RDN effectively reduced both office and ambulatory BP at 12 weeks post procedure in patients with resistant hypertension (RH). In this study, we further evaluated the efficacy of this technique in home BP control of 15 patients with RH. Based on the reduced use of anti-hypertension drugs following the procedure, the control rates of home BP (<140/90 mmHg) for the overall cohort were 60.0%/93.3%, 80.0%/100%, and 80.0%/100% at weeks 4, 8, 12, respectively, and 57.1%/90.91, 81.8%/100% and 90.9%/100% at weeks 4, 8, 12 for patients with normal baseline renal function. Additionally, 33.3% patients achieved the optimal morning BP target of ≤135/85 mmHg. No complications were reported intra- or post procedure. We present a simplified, unilaterally operated, contrast-free RDN technique that avoids renal artery injury in the management of RH.
Introduction
Resistant hypertension (RH) is diagnosed when individuals do not meet BP targets despite taking three antihypertensive medications, or when individuals achieve the BP target but require four or more antihypertensive medications1. RH is linked to a significantly higher risk of cardiovascular and renal adverse events2. Renal sympathetic denervation (RDN) -- from surgical sympathectomy or the current catheter-based RDN -- was demonstrated to be effective in the treatment of RH3,4,5.
Due to the invasiveness and severe side effects, surgical sympathectomy has been eliminated. There are still some limitations for catheter-based RDN, including contrast-dependence, potential renal artery injury, relatively lower cost-effectiveness, and the requirement of special catheter assistance6. These limitations highlight the need for improved RDN approaches. In recent years, other RDN techniques, such as CT-guided perivascular ethanol-mediated RDN, transurethral laparoscopic-based RDN, and laparoscopic-based perivascular unilateral RDN have been introduced, demonstrating effective BP reduction7,8,9,10.
The sympathetic ganglion, especially ganglia from T9-L2, are important components of renal sympathetic innervation and are convenient to target under CT guidance11,12. The smpathetic ganglion was the earliest target for RDN in surgery. A recent animal experiment has shown that the injection of ethanol in the celiac trunk ganglion resulted in significant BP reduction. High concentrations of ozone (18-30 µg/mL) promote an increase in the rates of apoptosis and neuroblast cell death13. Our previous trial showed that CT-guided ozone-mediated RDN effectively lowered office and ambulatory BP 12 weeks post procedure in RH patients14. In this study, we evaluate the changes in anti-hypertensive regimen and the effect of home BP control rate of this approach of RDN.
Protocol
This study was approved by the Guangzhou Red Cross Hospital Ethics Board (No. 2022-145-01), and written informed consent was obtained from all participants prior to enrollment. This single-arm clinical trial was designed and registered in Chictr.org.cn (ChiCTR2300071375).
1. Study design
NOTE: This was a prospective, single-arm clinical study aimed at observing the home BP control rate in patients before and after the procedure.
- Set the following inclusive criteria: age between 18 and 80 years; hypertensive patients with BP that remains elevated above 140/90 mmHg even with the simultaneous use of three antihypertensive medications from different classes, commonly including a diuretic; or patients whose BP achieves less than 140/90 mmHg on ≥4 antihypertensive medications.
- Exclude the following patients: diagnosed secondary hypertension; spinal deformities or infective; prior renal artery angioplasty or catheter-based denervation; previous lumbar internal vertebral disc radiofrequency ablation or sympathetic blockage; and a history of myocardial infarction, cerebral vascular accident, or transient ischemic attack within 3 months before enrollment; patients who did not upload the scales in a timely manner as required during the follow-up period.
- Evaluation of antihypertensive medication burden (AHMB)
- Assess the antihypertensive medication burden by counting the number of medication classes, disregarding the doses. When the criteria for medication reduction are met, consider discontinuing one class of medication, regardless of dosage, as reducing one burden. To maintain adherence and prevent unproven medication changes, have the follow-up team verify the medication plan with patients weekly and ensure those eligible for reduction are following the prescribed adjustments.
- Set the criteria for reducing antihypertensive drugs as systolic blood pressure (SBP) ≤ 110 mmHg on at least two consecutive measurements after the procedure.
- Home BP monitor
- To ensure the accuracy of home BP measurement, train all patients formally to measure their home BP at four different time points each day in a standardized manner: upon waking, at 10:00 AM, at 4:00 PM, and before bedtime. Request that patients log their home BP readings on a record form, which will be collected by the study team every week during follow-up.Define home BP control as SBP of ≤140 mmHg and a diastolic blood pressure (DBP) of ≥90 mmHg.
NOTE: An electronic automatic device was used to measure brachial artery BP.
- To ensure the accuracy of home BP measurement, train all patients formally to measure their home BP at four different time points each day in a standardized manner: upon waking, at 10:00 AM, at 4:00 PM, and before bedtime. Request that patients log their home BP readings on a record form, which will be collected by the study team every week during follow-up.Define home BP control as SBP of ≤140 mmHg and a diastolic blood pressure (DBP) of ≥90 mmHg.
- Safety: Report and record all possible adverse events via phone calls, messaging apps, or in the outpatient clinic. Potential complications include orthostatic hypotension, gastrointestinal dysfunction, dysuria, and male erectile dysfunction.
2. Preparation before the procedure (prone position training for patients in the ward)
- Have the patient assume a prone position on the bed, extending their arms parallel above the head.
- Place a pillow beneath the lower abdomen to flatten the lumbar curve, ensuring the back and buttocks are on the same level.
NOTE: Pillow placement may vary according to individual body types. - Carry out this exercise twice a day for 2-3 days with the aim of keeping the position stationary for at least 20 min.
3. Ozone-mediated renal denervation (in CT laboratory)
- Remove the patient's upper garment to expose the torso.
- Attach the electrodes and connect to an electrocardiogram monitor.
- Measure the supine blood pressure.
- Have the patient switch to a prone position, ensuring comfort and stability.
- For reference points on the body surface, place a metal wire on the midline of the torso (approximately at T12-L3 level) to act as a reference for the deviation distance from the midline of the body surface puncture point under CT guidance (Point C in Figure 1).
- Identify the puncture target
- Use a CT scanner to get anteroposterior and lateral images of the lumbar spine (range: S2 to T11) for vertebral counting and transitional vertebrae assessment.
- On the transverse images, identify the left renal artery origin level and determine the injection target point (Point A in Figure 1) at the anterolateral third of the vertebral right edge at this level.
NOTE: If the renal artery is directly below the transverse process at the same level, adjust the injection level to avoid the transverse process. - Record the corresponding transverse plane position.
- CT-guided puncture parameter measurement
- On the selected transverse image in step 3.6.2, identify injection target point A (Figure 1) at the anterolateral third of the vertebral side.
NOTE: The target point should be below the fascia of the ipsilateral psoas major muscle, ~2-3 mm away from the left renal artery. - Draw a line from A along the outer lateral border of the left psoas major. The intersection of this line with the body surface is the skin puncture point B, with the metal wire on the lumbar body surface corresponding to point C. Measure the length of AB (needle insertion depth), the angle between AB and BC (puncture angle Q), and the length of BC (lateral distance of the body surface puncture point from the midline (Figure 1)).
NOTE: Ensure that the needle remains entirely within the psoas major throughout its trajectory.
- On the selected transverse image in step 3.6.2, identify injection target point A (Figure 1) at the anterolateral third of the vertebral side.
- Surface puncture point positioning
- Adjust the bed to the recorded position in step 3.6.2. Activate the laser positioning line and mark two lines using a marker: one along the projection line (A line) and the other along the preplaced metal line on the body surface midline (B line). The intersection of these two lines is point C in step 3.5.
- Remove the metal wire and mark the puncture point B on line A according to the BC segment length measured in step 3.7.
- Puncture protocol
- Insert a 21 G needle with length markers at point B, puncturing at the predetermined angle to the predicted depth. Perform continuous 2 mm slice thickness scans around the puncture point ± 0.4-0.8 cm to confirm the needle tip.
NOTE: If resistance is encountered, indicating an excessive puncture angle and needle-vertebra contact, retract and readjust the puncture angle under CT guidance. - Connect a 10 mL syringe, ensure no blood or gas is aspirated, and then inject 2 mL of 10% ropivacaine. Use a 20 mL syringe to draw 10 mL of O2-O3 gas mixture from a medical ozone generator and inject slowly along the needle. Repeat the CT scan to show ozone distribution.
NOTE: The ozone concentration is 30 µg/mL.
- Insert a 21 G needle with length markers at point B, puncturing at the predetermined angle to the predicted depth. Perform continuous 2 mm slice thickness scans around the puncture point ± 0.4-0.8 cm to confirm the needle tip.
- After the procedure, ask the patient to lie in a supine position, and measure cuff BP every 5 min. Ensure that the monitoring in the CT room lasts for at least 20 min.
Results
Baseline characteristics:
Initially, 20 patients were selected. Two patients diagnosed with renal artery stenosis and one with sleep apnea syndrome were excluded, resulting in 17 patients eligible for inclusion. Of these 17 patients, two were unable to continue in the follow-up. Finally, 15 patients were included in this clinical observation, with an age of 65.1 ± 10.8 years. Six patients (6/15; 40.0%) had chronic kidney dysfunction and one (1/15; 5.9%) was on dialysis at the time of enrollment. Eleven patients (11/15; 73.3%) had been using antihypertensive medications for over 10 years. The 24 h mean SBP and DBP were 136.1 ± 20.9 mmHg and 72.1 ± 11.7 mmHg, respectively, with the AHMB of 4.1 ± 1.1.
Changes in anti-hypertensive drugs regimen after the procedure
One patient met the medication reduction criteria immediately after the procedure and did not take any antihypertensive drugs until 24 h later, when her BP increased gradually to more than 110/70 mmHg. The other six patients met the criteria during follow-up. At 12 weeks after the procedure, the percentage of patients needing more than four types of drugs to control their BP dropped from 87.8% to 53.3% for the whole participants and from 81.1% to 45.5% for those with baseline normal renal function (Table 1).
The home BP control rate post procedure
The control rate of home BP was calculated according to the BP threshold of ≤140/90 mmHg. The whole control rates of SBP and DBP were 60.0% and 93.3% at week 4, 80.0% and 100% at week 8, and 80.0% and 100% at week 12, respectively (Figure 2A). For patients with normal baseline renal function, only two (18.2%) and one (9.1%) patients failed to reach the standard of SBP < 140 mmHg at weeks 8 and 12, respectively (Figure 2B).
For each time spot, compared with the BP at 10:00 AM, 4:00 PM, and night, the morning BP remained significantly higher than others at 12 weeks post procedure (135.5 ± 8.9/81.6 ±6.4 vs 130.3 ± 8.9/79.2 ± 6.45, 130.5 ± 7.7/76.9 ± 6.1, 131.3 ± 8.0/77.5 ± 4.9). At 3 months follow-up (from week 9 to week 12), the BP control rates at each time point for all patients were 37.2%, 81.0%, 70.7%, and 86.0%, respectively (Figure 2C). However, for patents with normal baseline renal function, the control rates at the four time points were 55.6%, 90%, 77.8%, and 90.0%, respectively (Figure 2D). Among them, 33.3% of the morning BP reached the optimal target of ≤135/85 mmHg. No complications were reported during the procedure or in the period of follow-up.
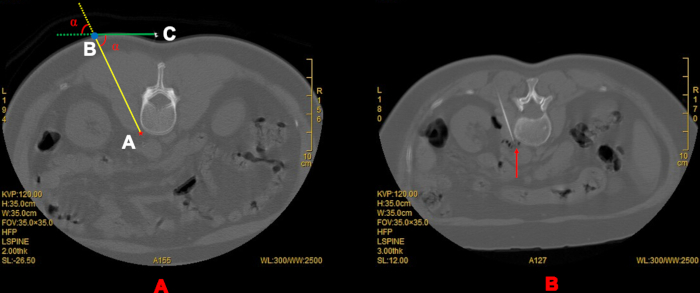
Figure 1: Identification of puncture point, depth, path, and angle. (A) Identify point A first. Next, draw line AB (along the outer lateral of the Psoas muscle) to get point B, and then measure the distance of AB as the puncture depth and regard the distance of BC as the lateral distance to the center line on the skin. The puncture angle (α) is the angle between line AB and line BC. (B) The diffusion of the gas mixture (Red arrow). A: point A (red star)-the target point. Point C (white spot)-the cross section of the prepositioned metal line. Please click here to view a larger version of this figure.
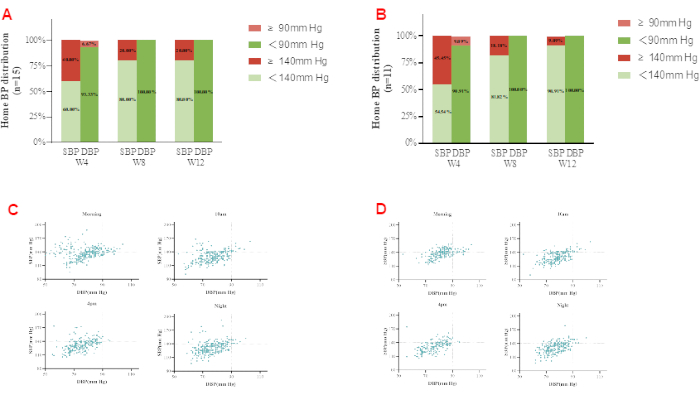
Figure 2: Home BP control rate. (A) The control rates of average SBP and DBP were 60% and 93% at week 4, 80% and 100% at week 8, and 80% and 100% at week 12. (B) The majority of patients (91%) with normal renal function achieved the BP control target at the 12 week follow-up. (C) The BP control rates at each time point for all patients were 37.2%, 81.0%, 70.7%, and 86.0%, respectively. (D) For patients with normal baseline renal function, the control rates at the four time points were 55.6%, 90%, 77.8%, and 90.0%, respectively. Please click here to view a larger version of this figure.
| Dosages of anti-hypertensive medication | Before Procedure | Week 4 | Week 8 | Week 12 |
| All (n = 15) | ||||
| 2 | 0 | 0 | 1 | 1 |
| 3 | 2 | 7 | 6 | 6 |
| ≥4 | 13 | 8 | 8 | 8 |
| With normal baseline Cr (n = 11) | ||||
| 2 | 0 | 0 | 1 | 1 |
| 3 | 2 | 6 | 5 | 5 |
| ≥4 | 9 | 5 | 5 | 5 |
Table 1: Changes in antihypertensive drug regimen after the procedure. After the procedure, the percentage of the patients who needed ≥4 types of antihypertensive drugs to keep BP < 140/90 mmHg dropped from 87.6% (13 of 15) to 53.5% (8 of 15). For patients with normal renal function at baseline, after the procedure, the percentage of the patients who needed ≥4 types of antihypertensive drugs to keep BP < 140/90 mmHg dropped from 81.8% (9 of 11) to 45.5% (5 of 11). None of the results above meets statistical significance in Fisher's exact test. Cr: Creatinine.Abbreviation: Cr = Creatinine.
Discussion
Our previous study demonstrated that ozone-mediated RDN significantly reduced in-hospital, office, and ambulatory BP, as well as antihypertensive medication use. The BP reduction was rapid and persisted through the 12 weeks follow-up. Additionally, we observed that the BP-lowering effect was particularly noteworthy in patients with normal baseline renal function14. In this study, CT-guided ozone-mediated RDN showed the effect of improved home BP control for patients with RH.
Given that the anatomical characteristics of the sympathetic innervation of the kidneys serve as the fundamental basis for this technique, it is of utmost importance to ensure precision in the injection process. Consequently, we strongly emphasize that the injection target point ought to be positioned as closely as possible to the site where the left renal artery originates from the descending aorta, thereby maximizing the technique's efficacy and accuracy in alignment with its anatomical underpinnings. Therefore, an initial CT scan thickness of 1 mm is recommended to fully display the renal arteries and identify any accessory renal arteries, which may be related to poor BP-lowering response. If the left renal artery origin is located directly below the vertebral transverse process, the target level should be adjusted upward to avoid the transverse process. It is imperative not to select a lower target level. This is because the lumbar sympathetic ganglia that innervate the kidneys are generally situated at the T8-12 and L1-2 levels11. Opting for a lower level significantly increases the likelihood of missing the key anatomical components of the renal sympathetic system, thereby undermining the effectiveness of the procedure.
When identifying the target point, it is crucial to consider the anatomical arrangement of the sympathetic nerve chain, which extends along both sides of the vertebrae. Consequently, the optimal target point should be precisely situated at the anterolateral one-third portion of the lumbar vertebra. Given that the lumbar psoas major artery usually courses alongside the vertebrae, the puncture needle should be accurately placed approximately ~1 mm lateral to the vertebral edge. Moreover, the selection of the target point should not only be in close proximity to the lumbar sympathetic ganglia but also ensure that the puncture penetrates the fascia of the psoas major muscle. Failure to meet these criteria may result in the ozone being trapped within the psoas major muscle, thereby preventing it from making contact with the ganglia and potentially diminishing the effectiveness of the procedure.
CT imaging reveals two additional anatomical structures involved in renal sympathetic innervation in the vicinity of the target point: the aortorenal ganglion, located at the angle between the aorta and renal artery, and the sympathetic nerve fibers that are embedded within the renal artery wall. Therefore, a lower target point allows the ozone to potentially reach one or all three relevant anatomical targets -- the lumbar sympathetic ganglia, the aortorenal ganglion, and the sympathetic nerve fibers on the renal artery wall -- resulting in a more comprehensive denervation. However, care must be taken to avoid any renal artery injury. To minimize this risk, we strongly recommend positioning the injection point 2-3 mm above the renal artery.
Once the ideal target point has been accurately determined, a line should be drawn upward direction along the lateral margin of the ipsilateral psoas major muscle to identify the surface puncture site. This process helps to ensure that the entry point is as lateral as possible while optimizing the puncture angle. It is crucial to avoid a trajectory that exceeds the lateral boundary of the psoas major muscle, as this may damage the renal fascia. In female patients, and in some males with relatively underdeveloped psoas major muscles, the puncture angle is generally narrower, sometimes approaching 90°. This steep angle increases the probability of the needle contacting the transverse process, adding complexity and requiring additional care.
In this study, puncture was performed solely on the left side. This approach is anatomically advantageous because the abdominal aorta usually lies to the left of the spine, increasing the probability of ozone reaching both the aortorenal ganglion and the outer membrane of the renal artery. in contrast, the inferior vena cava typically runs along the right side of the abdominal aorta, making right-sided puncture more hazardous due to the heightened risk of vena cava injury.
When the patient is placed in a prone position, ensuring that the lumbar spine remains at a consistent level during CT localization and surface projection. Since the renal arteries in adults are usually located at the L1-L2 vertebral level, it is critical to avoid substantial angular deviations between L1 and L2 vertebrae. We recommend that patients remain in the prone position for at least 20 min to ensure stability, as the CT measurement and procedure usually take 5-20 min. Maintaining a fixed position throughout the procedure is critical for a successful and safe puncture because even the most minimal patient movement can cause the puncture needle to deviate from the carefully calibrated CT-guided trajectory.
There are several limitations to this study. First, it was an open-label, observational feasibility study without a sham-control group. The sample size was limited, and the follow-up duration was limited to 3 months. Thus, a randomized controlled trial with a larger cohort and extended follow-up period is warranted to more robustly assess the safety and efficacy of this technique. Further mechanistic investigations are also needed to validate our findings and enhance our understanding of the underlying pathways. Given that both sympathetic and vagal nerves regulate blood pressure via distinct pathways but are anatomically colocalized, accurately distinguishing and selectively targeting these fibers remains technically challenging-a common limitation of current RDN techniques. Therefore, it is difficult to definitively attribute the observed blood pressure reduction following ozone injection solely to selective sympathetic modulation, as inadvertent vagal nerve involvement cannot be entirely excluded. In addition, this study used medication burden as one of the surrogate markers for efficacy. While medication burden can provide useful insights, it has notable limitations. It may not fully reflect treatment efficacy, as it does not account for factors such as patient adherence, medication interactions, or the actual therapeutic impact on disease progression. In future studies, we plan to incorporate standardized efficacy scores (e.g., WHO Defined Daily Dose [WHO-DDD] or the HARC index) to provide a more comprehensive assessment of treatment outcomes.
Disclosures
The authors have no financial conflicts of interest to declare.
Acknowledgements
This study is funded by Guangzhou Municipal Science and Technology Bureau (2023A03J0984 and 2024A03J0654).
Materials
| Name | Company | Catalog Number | Comments |
| CT scanner | General Electrics, Hi Speed ZX/I. USA | ||
| Graduated measuring tape | no specified brand | ||
| Marker pen | no specified brand | ||
| Medical ozone generator | Medozon compact, Herrmann Apparatebau GmbH. Germany | ||
| Metal wire | no specified brand | ||
| Peit needle | Hakko Co., Ltd. JAPAN | 21 G x 150 mm | |
| Ropivacaine Hydrochloride Injection | AstraZeneca AB | 100 mg/10 mL | |
| Single-use puncture pack | no specified brand | containing sterile cotton swabs, sterile gauze, sterile surgical drape, a 5 mL syringe, and a 20 mL syringe. |
References
Reprints and Permissions
Request permission to reuse the text or figures of this JoVE article
Request PermissionThis article has been published
Video Coming Soon
Copyright © 2025 MyJoVE Corporation. All rights reserved