Method Article
Standardization of Basket Use in Sialendoscopy: A Ten-Year Retrospective Study
In This Article
Summary
We present the standardization of the basket use in sialendoscopy for obstructive sialolithiasis in a consecutive ten-year series of patients with obstructive salivary gland, describing localization, stone evaluation, size estimation, choosing basket type, and choosing approach technique (Frontal, Side-to-Side, Back-to-Forward) to achieve a high success rate in its removal.
Abstract
Sialolithiasis is a common cause of obstructive salivary gland disease, occurring in both submandibular and parotid glands. The treatment has evolved with the introduction of Sialendoscopy and micro-instruments (baskets, wires, and balloons), which allow intraductal manipulations, including stone removal and strictures, to be dilated. Nowadays, it is the main option for effectively treating these obstructive conditions, leading to improvements in overall quality of life. The objective of the present 10-year retrospective review is to standardize the basic steps involved in successfully removing intraductal sialolithiasis with a Basket instrument.
A consecutive ten-year series (January/2014 to June/2024) of patients with obstructive submandibular and parotid glands due to sialolithiasis who underwent sialendoscopy using a basket successfully removed were analyzed. The procedure was conducted following the standards; all interventions were video-recorded and performed by the same surgical team using a semi-rigid modular sialendoscope (1.3 mm/1.7 mm diameter) with working channel, salivary probes, dilatators, different baskets (0.4 mm diameter and 3, 4 and 6 wires) for stones and dilatations, using some steps previously reported.
In 10 years, we have performed 224 sialendoscopy due to salivary gland obstructive disease, 84.4% from sialolithiasis. The successful sialolith removal with the basket was performed using pure sialendoscopy (PS-study group) in 132 (69.8%) patients: 79.5% female patients, mean age 44.8 years; 68.9% in the submandibular gland, 65.9% single stones, with 0% major complications. The basic steps were a) how to localize; b) to evaluate (mobile/hard/single stone); c) to estimate sialolith size; d) to choose basket type; e) to choose approach technique (A: Frontal:9.1%, B: Side-to-Side: 35.6%, C: Back-to-Forward: 55.3%). All sialoliths were completely removed, and the patients recovered uneventfully. This article details the standardization of the use of basket in removing ductal stones during sialendoscopy, which is necessary to achieve a high success rate in its removal.
Introduction
The obstructive salivary gland disease is due to sialolithiasis in almost 60% of cases, the strictures, mucoid debris, and anatomic ductal abnormalities among the other causes1. Nearly 80%-95% of sialolithiasis cases occur in the submandibular gland and 5%-20% in the parotid gland2. This condition has also been proven by image studies, usually ultrasound, computed tomography, or eventually magnetic resonance3,4,5.
Their treatment has evolved in the last 25 years since the introduction of sialendoscopy with very thin semi-flexible endoscopes and adequate miniaturized related instruments like forceps, baskets, wires, and balloons. These new instruments allowed intraductal manipulations, including stone removal, dilatation of strictures, and cleansing of mucus plugs during sialendoscopy2. In some special cases, all these procedures can be used in combination with minimally invasive external approaches6.
Nowadays, sialendoscopy is the main option for effectively treating these obstructive conditions, leading to improvements in overall quality of life7,8,9. Nevertheless, no article has clearly shown the standardized basic steps to follow in the sialolithiasis treatment through sialendoscopy using the basket instrument.
The basket instrument use during sialendoscopy is a well-established technique for the retrieval of salivary stones, and it must be done inside the duct, a clear advantage over the open surgical techniques once this last involves the mucosal and skin incisions, nerve manipulations, and sometimes salivary gland excision10,11,12. In this point of view, the knowledge of how to properly use the basket in a patterned way will help the assistant surgeon to adequately and safely treat these salivary obstructive conditions, saving surgical time, saving the salivary gland, and avoiding potential complications2,13,14,15,16.
The basket use procedure typically involves the following intuitive steps: Identification and access of the salivary duct through a sialendoscope, stone identification, introduction of the basket through the sialendoscope, opening of the basket, stone capture, and retrieval15,17,18. These steps are usually done with a relatively good success rate in experienced hands but have potentially hardazous complications, like avulsion of the salivary duct, gland swelling, salivary fistulas, stuck basket inside the duct, salivary ducts perforations (false rout - "via falsa"), traumatic ranulas, and the lingual nerve paraesthesia14,16.
There is also no detailed article describing the standardized intraductal use of the basket instrument during the sialendoscopy in a series of patients for a safe and high success rate, an apparently simple task that is still done in intuitive mode. Some studies have described random and non-standardized movements of the basket to engage the stone in the region of the hilum of Stensen's duct, but without mentioning the success rates for each maneuver or how it has been used in other parts of the main duct19. The rationale and correct application of standardized basket use for the removal of salivary stones will allow the adequate treatment of sialolithiasis with sialendoscopy while reducing operative time and related complications.
The present method proposed by the authors should be used whenever possible in any situation where intraductal salivary stones can be removed mainly via pure sialendoscopy or sometimes in association with a planned combined procedure.
In the protocol below, we used these important definitions of approach techniques.
Type A: Frontal - The tip of the basket is located against the anterior part of the sialolith, and the opening of the basket threads is made anterior to the sialolith. By instilling a sterile physiological 0.9% saline solution, the stone can move anteriorly into the basket, becoming trapped.
Type B: Side-to-Side -The tip of the basket is located next to the sialolith, and during the opening of the basket threads, the position is on the side of the sialolith and by instilling sterile physiological 0.9% saline solution, the stone can move laterally into the basket, becoming trapped.
Type C: Back-to-Forward -The tip of the basket is located posterior to the sialolith, and the opening of the basket wires is made posterior to it, bringing it anteriorly to the sialolith to trap it inside the basket
The main objective of this 10-year retrospective review is to standardize the basic steps involved in successfully removing intraductal sialolithiasis with the basket instrument, facilitating the handling of the instruments and the basket during sialendoscopy, making the procedure highly safe and successful.
Protocol
All procedures were conducted under institutionally approved protocols, in accordance with the Institution Human Research Ethical Guidelines, and approved by the Ethics Committee. Informed consent was obtained from the patients to film the surgery for educational purposes before starting the process.
NOTE: The materials suggested to be used are semi-rigid modular sialendoscope, as listed in the Table of Materials, with a diameter of 1.3 mm or 1.7 mm and with the working channel; salivary probes, conic dilatators, bougies, baskets for stones, dilatator balloons, silastic stents, and sterile physiological 0,9% saline solution.
1. Preoperative procedures
- Once in a sterile field, check the sialendoscopes and support instruments by carefully inspecting them and verifying the integrity of the material. (Figure 1A,B).
- Inspect and check the basket operation by testing the opening of the wires manually outside the duct system, following the instructions in the manufacturer's manual. (Figure 1C).
- Inspect and check the operation of the inflated balloon by filling the balloon with sterile physiological 0.9% saline solution, according to the volume recommended by the manufacturer, which varies from 0.2-0.4 mL, always following the instructions in the instruction manual.
- Inspect and verify the operation of the fiber optic cables connecting them to the video rack lighting system, initially maintaining a low light intensity, about 50% of the possible, and connecting the other end to the fiber optic plug of the sialendoscope (Figure 1D).
- Inspect the video camera cable and connect the video camera of the video set, properly protected with sterile wrap, to the video connector of the sialendoscope.
- Inspect and check the image on the video monitor screen for the presence of light and the quality and image formation while trying to read the wire packing label.
- Adjust the camera zoom to focus the image by rotating the video image adjustment to eliminate the presence of "honeycombs" in the image seen on the monitor screen. Use the label on the wire packaging to ensure the letters are seen and have acquired better image quality.
- Insert the optical fiber into the sialendoscope if using the "sheets" for sialendoscopy, adjusting it so that it is correctly adapted to the material. Follow the same steps above to calibrate the video set.
- Locate the irrigation channel of the sialendoscope caudally, with the optical fiber located in the middle of the instrument and the working channel located cranially. Use the label on the wire packaging to correctly position the "north" of the sialendoscope on the image screen.
- Connect the saline solution equipment containing full sterile physiological 0.9% saline solution to the irrigation channel, checking that no air bubbles have formed inside that will interfere with the formation of the video image in the ductal system.
- Check and mark the correct side of the patient's neck or face to do the sialendoscopy with a washable surgical pen marker; do the same on the salivary gland on which the sialendoscopy is to be performed (Safe Surgery Protocol).
- Perform all the operations under general anesthesia, with the use of salivating stimulators like neostigmine as the surgeon's choice: adult single dose of neostigmine 0.5-2.5 mg (0.05-0.07 mg/kg) to be administered simultaneously (in separate syringes) with atropine sulfate 0.6-1.2 mg (0.02 to 0.03 mg/kg) by slow intravenous (IV) injection over 1 min, with caution, in accordance with the anesthesiologist preferences and following the manufacturer data sheet.
- Perform all the steps above before starting the anesthetic procedure in the operating room. Ensure all interventions are video-recorded and performed by the same surgical team for diagnostic and therapeutic procedures.
2. Sialendoscopy technique
- Place the patient in the supine position under general anesthesia with the orotracheal tube located on the contralateral side of the gland for sialendoscopy.
- Perform the routine mouth asepsis and antiseptic following the rules with proper oral 0.2% chlorhexidine mouthwash and covering the sterile surgical field, ensuring that the side on which sialendoscopy is to be performed is exposed.
- Check the sialendoscope again as soon as the sterile field is ready on the patient, making the necessary adjustments: to the white balance, press the WB button on the camera or in the video device located in the video set; do the same to adjust the zoom and focus on the camera.
- Check again for the spatial orientation of the optical instrument, which is necessary for safe intraductal navigation.
- Put the open-mouth gag on the contralateral side, adequately exposing the papilla of the salivary gland to be submitted to sialendoscopy, either submandibular or parotid gland.
- Dilatate progressively the salivary gland papilla with dilatators until it fits the adequate size of the sialendoscope to allow the insertion of the sialendoscope and proper visualization of the duct (Figure 2).
- Introduce delicately the sialendoscope inside the main duct, and connect a 20 mL syringe filled with sterile 0.9% physiological saline solution or sterile isotonic water to the irrigation system connected to the sialendoscope irrigation system.
- Slowly and carefully inject small portions, with low pressure, sufficient volume of the sterile 0.9% physiological saline solution to distend the duct that will be visualized on the video monitor screen.
- Navigate gently into the duct once it is distended, allowing the sialendoscope to enter it effortlessly without major maneuvers and twists (Figure 3).
- Inspect the main duct, secondary and tertiary ducts as possible, in detail with sialendoscope, cleaning from mucus plugs using the saline solution irrigation instilled by the syringe in small amounts as much as necessary to clean it, which should not usually exceed the total volume of 60 mL in the entire procedure, taking into account the loss (exit) of saline solution into the oral cavity around the sialendoscope in the salivary papilla.
- Locate the stone(s) inside the duct after cleaning it, and be prepared to perform the salivary stone capture maneuvers.
3. Basic steps on standardization of basket use in sialendoscopy
- Initial inspection:
- Exam with the sialendoscope all duct extensions during this initial phase, looking for stenosis presence and evaluate the stenosis along the main, secondary, and tertiary ducts.
- Note the appearance of the duct stenosis and its location, and estimate its size by comparing it to the main duct. (Figure 4). Also, observe the stone presence after the stenosis (if any) and how the saliva is affected by the last (milky or clear appearance) (Figure 5).
- Localization of sialolithiasis
- Inspect the main duct, secondary, and tertiary ducts, looking directly for stones after the initial inspection, and make notations where the stone is located in the main duct, secondary, or tertiary ducts (Figure 6A, B).
- Sialolithiasis estimation
- Size: Observe the sialolith carefully and make notes of the size of the stone(s) (i.e., all duct diameter or lesser than duct diameter) (Figure 7A, B).
- Number: Identify if the stone(s) are single or multiple, trying to establish a plan of treatment (single or multiple attempts) (Figure 8A, B).
- Mobility: Move the sialendoscope and flush the sterile 0.9% physiological saline solution carefully at the same time to observe and evaluate the mobility of the stones, recording their characteristics as fixed/little mobility or mobile stones (floating along the duct).
- Consistency: Identify and try to presume the stone's consistency by its physical appearance and/or touch it gently with the sialendoscope and try to feel it by the touch, as hard or soft.
- Basket type selection: 3, 4, 6 wires: Choose the appropriate basket based on observations of steps 3.2 and 3.3 to achieve a higher chance of trapping the stone. Note that small stones will need more wires to facilitate the catch maneuver, and bigger and small mobility stones will require fewer wires (Figure 9A, B).
- Approach technique
- Type A: Frontal:
- Choose the Type A-frontal approach after complete evaluation as described above by putting the tip of the basket against and very close to the anterior part of the sialolith (Figure 10A).
- Open the wires gently, carefully flush the saline solution, and try to trap the stones as they move the saline solution into the basket. (Figure 10B). This approach is ideal for mobile, smaller and occasionally soft stones, using the 4 to 6 wires basket.
- Type B: Side-to Side:
- Choose this type of approach for a relatively mobile, single stone that is smaller than the size of the duct. To do this, place the tip of the basket next to the stone, and by doing so, the wire will be located on the side of the sialolith. (Figure 11A).
- Carefully flush the sterile 0.9% physiological saline solution with the soft movement of the open basket to dislodge the stone and catch it with the basket. (Figure 11B).
- Type C: Back-to-Forward:
- Choose this type of approach in cases of all-duct size stones with hard consistency or single stones with little mobility.
- Put the tip of the basket posterior to the sialolith (Figure 12A), and make sure to open the wires posterior to it. After this, slightly bring the wires of the basket anteriorly, and at the same time, gently flush the sterile 0.9% physiological saline solution (Figure 12B).
- Finally, after the wires are around the stone, secure the stone, pulling the basket wires. (Figure 12-C).
- Type A: Frontal:
- Final inspection: Make the final duct inspection before finishing the procedure; it is when the main duct, secondary, and tertiary ducts are evaluated afresh, looking for residual stones and stenosis. Be prepared to solve any other problem again and repeat the above steps if necessary (Figure 13).
- Remove the endoscopic system and evaluate the papilla or duct stent necessity, putting it in appropriate extension and orientation and fixing it to the mucosa with a non-absorbable suture.
- Finish the endoscopic procedure, stop the video recording, and allow the patient to wake up safely. Evaluate the face and neck again looking for major swelling of the salivary gland to prevent airway distress. In this case, allow to recover more time than conventional in the recovery room properly monitored.
4. Pos-operative procedures
- Keep the patient in-hospital for 1 day, as intense pain and swelling in the salivary gland area occurs in some patients. Treat with analgesics, antibiotics (usually cefazoline), and a soft diet.
- Mobilize the patient as soon as possible following the procedure.
- Discharge the patient on the following day if there are no complaints.
Results
In 10 years, we have performed 224 consecutive sialendoscopies due to salivary gland obstructive disease. Of these, 189 (84.4%) were caused by sialolithiasis. The successful sialolith removal with Pure sialendoscopy only (PS-study group) was done in 132 (69.8%) patients, all with uniglandular disease, utilizing the above-mentioned protocol.
In the PS study group (n = 132), there were 105 (79.5%) female patients, with a mean age of 44.8 years (ranging from 15 years to 84 years); the endoscopic stone extraction index was 100%, and 68.9% of stones occurred in the submandibular gland (Table 1).
As shown in Table 2, almost 65.9% consisted of single stones, with no major complications during the sialendoscopy, no cases of stuck baskets occurred, and the average sialendoscopy mean time duration was 62 min (Table 2).
Table 3 describes the basic steps and the important results (Table 3):
a) localizing stone: 73.5% in the main duct.
b) stone evaluation: 100% were mobile and of hard consistency; 65.9% were single stone.
c) estimation of sialolith size: mean size of 4.3 mm (2.0-5.5 mm).
d) basket type: 25.8% were 3 wires, 68.9% were 4 wires, and 5.3% were 6 wires baskets.
e) Approach technique used: A: Frontal: 9.1%, B: Side-to-Side: 35.6%, C: Back-to-Forward: 55.3%.
f) Approach Technique X Stone size: we used the Type A and B techniques mainly for smaller than duct-size stones: 59 (44.7%) and Type C technique for all duct-size stones: 73 (55.3%)
All stones were trapped effectively with the basket. Papilla stenting was necessary primarily in all duct-size stones: 73 (55.3%) patients, when the diameter of the stone was extremally bigger than the papilla ostium, being necessary to cut the papilla; however, duct stenting or papilla stenting was necessary in 98.4% of the cohort as the mean size of stones was 4.3 mm (Table 2 and Table 3). Some authors have found the same findings regarding stent use for salivary obstruction in sialendoscopy due to stones, but in a small number of patients; others have used it only in stenosis situations20,21. All patients recovered uneventfully postoperatively and were discharged the next day.
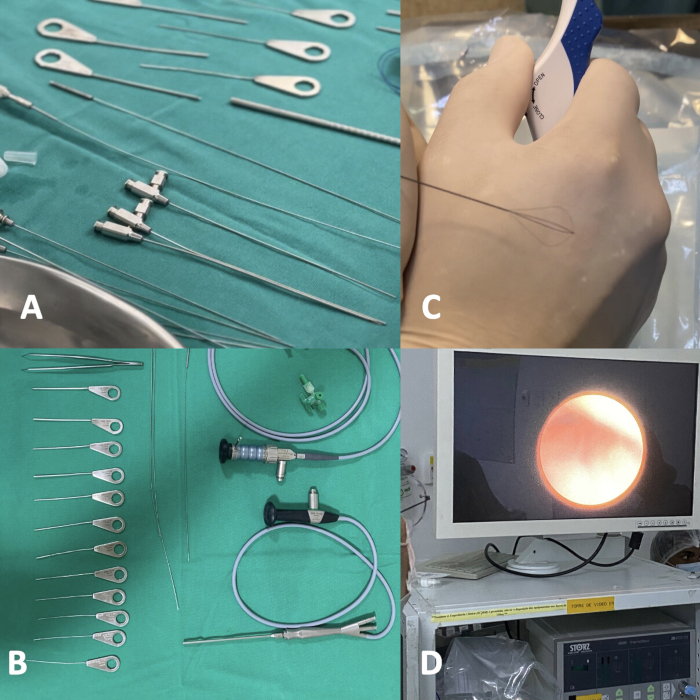
Figure 1: Checking the materials for sialendoscopy. Probes, basket, ballon, video camera, optic cables, video set. Please click here to view a larger version of this figure.
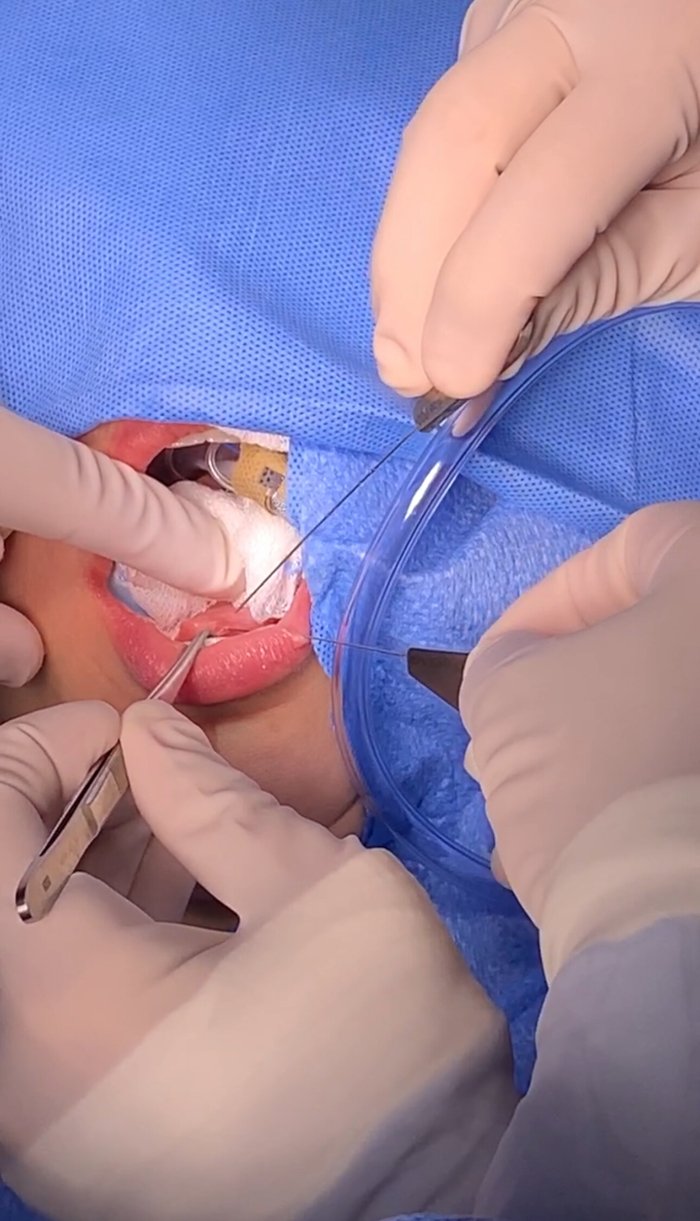
Figure 2: Papilla dilatation with probes. The papilla is dilated with the help of probes. Please click here to view a larger version of this figure.

Figure 3: Navigation inside the duct with Sialendoscope. Navigation inside the duct is performed with a sialendoscope and an irrigation system. Please click here to view a larger version of this figure.
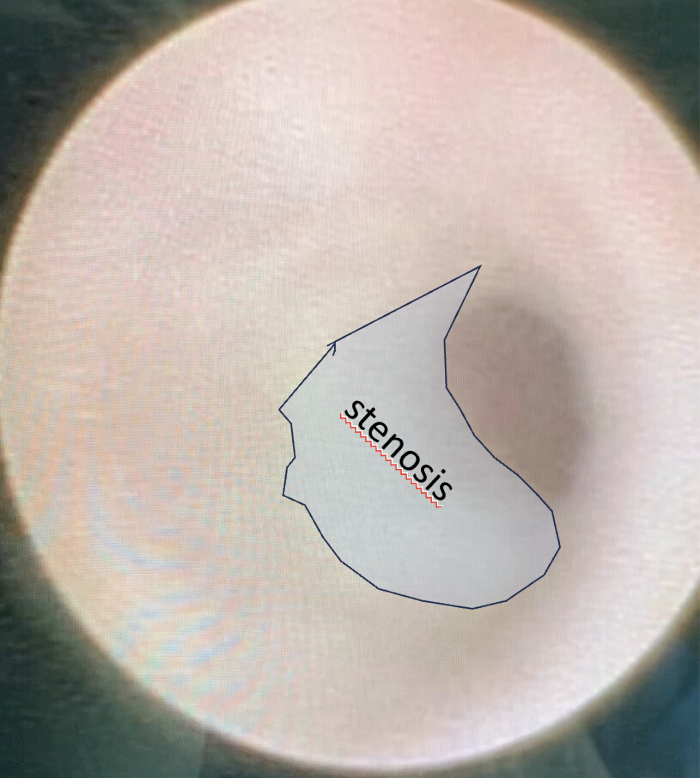
Figure 4: Stenosis appearance inside the duct during the initial inspection of sialendoscopy. Note the appearance of stenosis inside the duct and its location and try to estimate its size. Please click here to view a larger version of this figure.
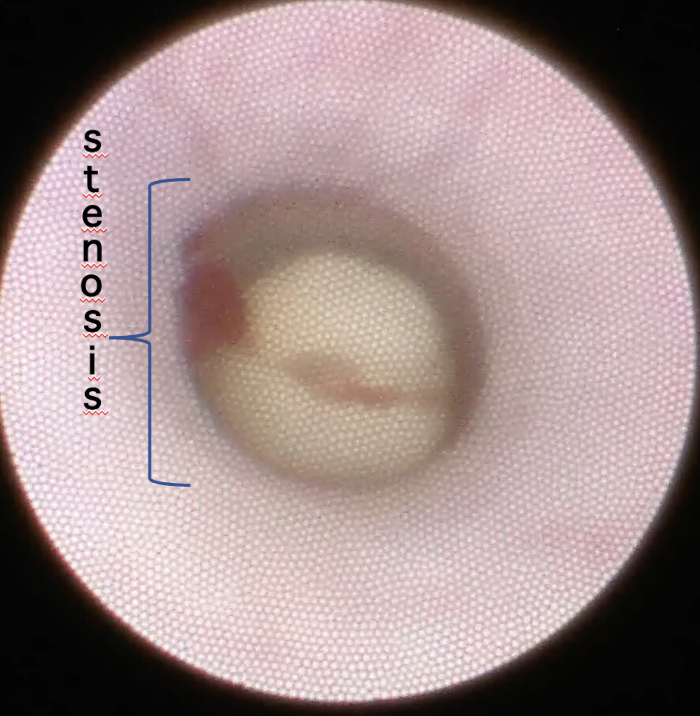
Figure 5: Salivary stone after stenosis inside of the duct during the initial inspection of sialendoscopy. During the initial inspection, note the stone just behind the stenosis in the duct, its location and size. Please click here to view a larger version of this figure.

Figure 6: Localization of sialolithiasis. Inspection of the main and secondary ducts, looking for salivary stones. Note the presence of stones in the (A) main and (B) secondary ducts. Please click here to view a larger version of this figure.
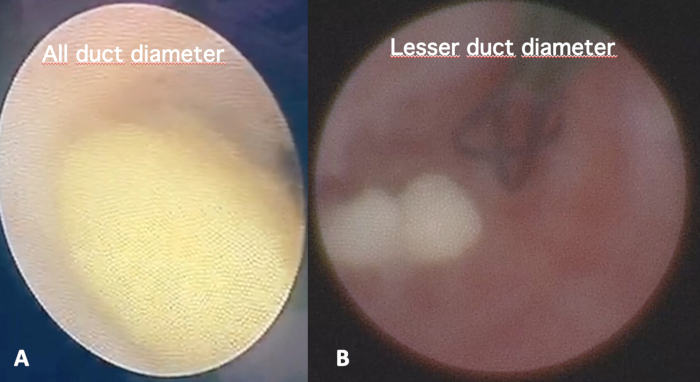
Figure 7: Sialolithiasis estimation size. Estimation of the intraductal sialolithiasis size comparing it to the main duct at close view, classifying it in (A) all duct diameter or (B) lesser than duct diameter. Please click here to view a larger version of this figure.
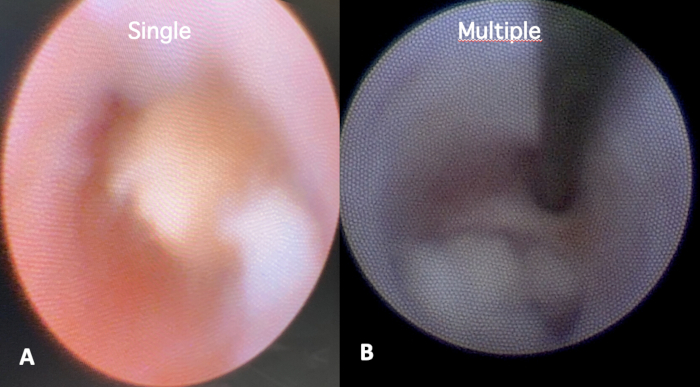
Figure 8: Sialolithiasis estimation number. Identification of the number of stones inside the duct, classifying it as (A) single or (B) multiple. Please click here to view a larger version of this figure.
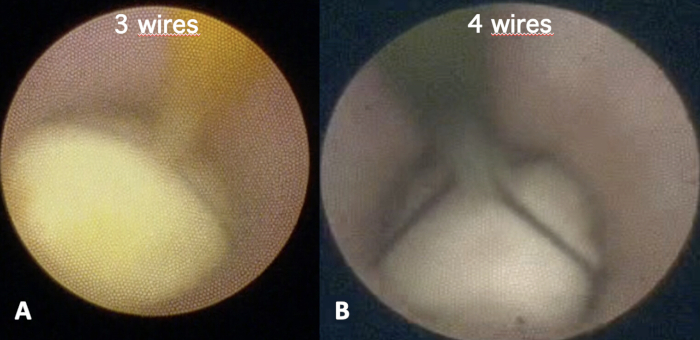
Figure 9: Basket type selection. Choose the appropriate basket: (A) 3 wires; (B) 4 wires or 6 wires to achieve a higher chance of trapping the stone. Please click here to view a larger version of this figure.
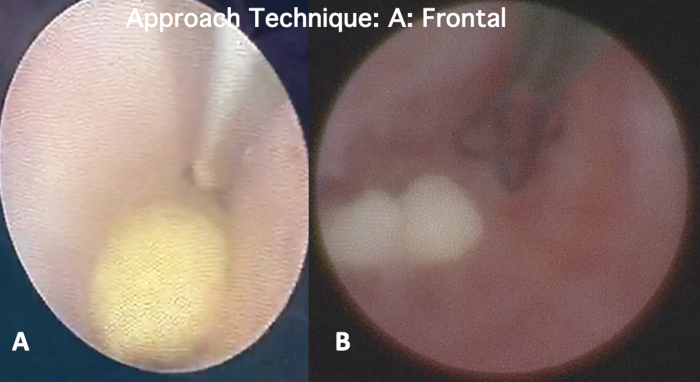
Figure 10: Type A: Frontal approach. This approach is performed by putting the tip of the basket against and very close to the anterior part of the (A) stone and (B) opening the wires gently at the same time, carefully flushing the saline solution, trying to trap the stone. Please click here to view a larger version of this figure.

Figure 11: Type B: Side-to-Side approach. In this approach, the tip of the basket is placed next to the stone, and (A) the wire will be on the side of the sialolith. (A) Flushing saline and moving the open basket will move the stone into the basket. Please click here to view a larger version of this figure.

Figure 12: Type C: Back-to-Forward approach. In this approach, the tip of the basket is placed (A) posterior to the stone, then (A) brought anteriorly with open wires. (C) After the wires are around the stone, secure the stone, pulling the basket wires. Please click here to view a larger version of this figure.
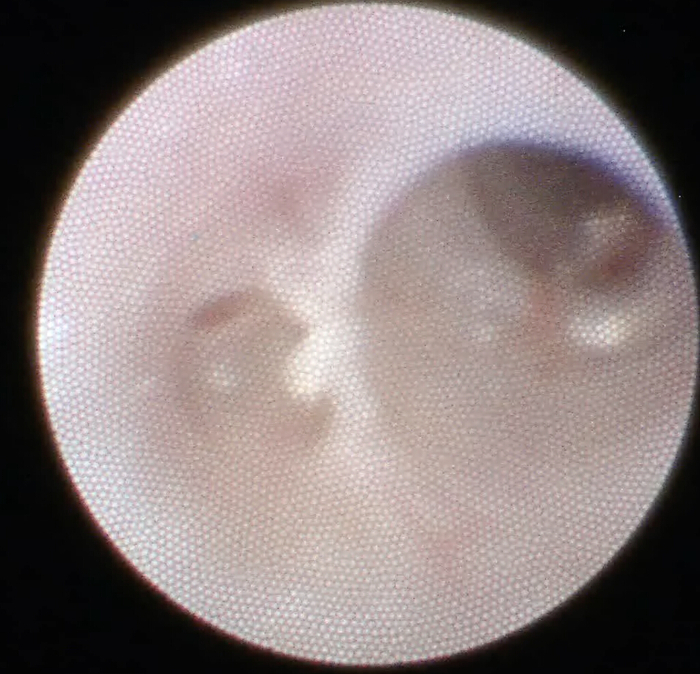
Figure 13: Final inspection. Before finishing the sialendoscopy, always inspect the duct system at the end of the procedure, certifying that it is clear and clean. Please click here to view a larger version of this figure.
Table 1: Pure sialendoscopy (PS) group clinical data showing the gender, age, diagnosis, and procedures carried out. Please click here to download this Table.
Table 2: Pure sialendoscopy (PS) Group clinical data of stones, postoperative complications, and sialendoscopy duration time. Please click here to download this Table.
Table 3: Clinical endoscopic characteristics of basket use in the PS group. Please click here to download this Table.
Discussion
Currently, in the general population, despite the heterogeneity of the studies, nearly 60-70% of obstructive salivary gland disease is caused by sialolithiasis. Nowadays, sialendoscopy is the main treatment option, removing stones and strictures and becoming the gold standard to treat these conditions as it restores the quality of life, keeping a functioning salivary gland intact1,7,22.
However, in the cases of sialolithiasis, there are some difficulties in the procedure, in all steps, until the final stone trapped is taken out to the mouth. Therefore, adequate intraductal manipulation with the basket is necessary to achieve a high success rate in sialolithiasis removal. However, there still exists a lack in the current medical literature on adequately describing how to perform it6,23,24,25.
This 10-year retrospective review, with a substantial number of patients and procedures, looked to standardize the basic steps involved in successfully removing intraductal sialolithiasis with a basket instrument.
The systematized protocol proposed here allowed a high success rate (100%) in sialolithiasis removal, preserving the salivary gland with no major complications, like other studies6,24. However, some studies have reported a high number of minor and major complications index, like canal perforations, readmissions due to persistent gland swelling or pain, lingual nerve injuries, and even salivary gland resection26,27.
In the cases included in this study, there have been no occurrences of equipment failure (malfunctions) during the sialendoscopy, maybe due to the rigid preoperative checklist protocol that detected and solved it before starting the procedure. However, malfunctions are relatively common, as shown in the literature25,28. So, all equipment must be checked to avoid related complications or failure intraoperatively, and this protocol will probably help to standardize it.
We have found that most stones have hard consistency (100%), and the majority of single stones (65.9%) are localized in the submandibular gland (69.9%), consistent with the literature29,30. Of note, there was a female predominance (79.5%) with a mean age of 44.8 years, comparable to current literature. Thus, the data here shows that this protocol could be easily applicable and reproducible in the population with salivary stones. The limitations of the technique are few and occur in patients with fixed salivary stones, in those who have developed complications such as a stuck basket or duct perforations, and in those where the team of assistant surgeons has no experience (beginners) with sialendoscopy.
Using the above-described protocol, we clearly have defined the basic steps on how to localize, evaluate (mobile/hard/single stone), estimate sialolith size, and select the basket type that we have applied in all patients without difficulties. The technique can be modified according to the surgeon's preferences or as they gain experience when starting to use it on their patients; however, until now, no literature data has been presented focusing specifically on this topic of sialendoscopy.
Most importantly, we have standardized the way to choose the approach technique to the basket use with respect to existing methods, defining it as Type A: Frontal, Type B: Side-to-Side, and Type C: Back-to-Forward, where the surgeon assistant can use during the sialendoscopy, sometimes varying from one to another type to capture the stone, as demonstrated in Table 3. The most successful procedure in this study is the Type C approach, followed by the Type B approach (Table 3), with no data in the literature to compare it.
The papilla stenting was necessary primarily in all duct-size stone patients (55,3%). The main criteria were that every time when we needed to open the papilla to retrieve the stone since we destroyed the natural muscle fibers of the anatomic papilla, the papilla cut could evolve into future papilla stenosis. Stenting it could prevent this complication. This has also been observed in another study20. Unfortunately, there are no sufficient similar findings in the literature to allow comparison.
The data provided in this study proved the safety and reliability of this protocol and could help others to improve their sialendoscopy practice. Until now, in sialendoscopy literature, there have been some meta-analyses, reviews, and systematic reviews, but no data has been reported on this type of standardization protocol improving the safety of the technique2,31,32,33,34.
As mentioned above, all sialoliths were completely removed without difficulties and with no complications. The patients recovered uneventfully, but one possible bias and limitation of the technique is that our team is highly trained to perform sialendoscopy. This can be hard in the initial cases for the beginner in practice as it is necessary to achieve the appropriate learning curve, as demonstrated in the literature2,35,36,37. Nevertheless, on the contrary, if there are no attempts to use the technique safely, the learning curve will not be completed. This is where the protocol proposed will be very useful in creating a safety protocol for beginners using the sialendoscopy technique. Moreover, more studies must be done to validate and confirm the findings reported in this study.
Standardization of the use of basket in sialendoscopy for obstructive sialolithiasis is necessary to achieve a high success rate in its removal. This method details the standardization of basket use in removing ductal stones during sialendoscopy. Our findings support the safe and effective use of the standardized basket in treating obstructive sialolithiasis in sialendoscopy, becoming an opportunity to standardize the technique worldwide to allow future prospective studies to be carried out.
Disclosures
The authors declare no conflict of interests
Acknowledgements
No acknowledgments
Materials
| Name | Company | Catalog Number | Comments |
| Baskets for stones | Humanna medical, Brazil | https://www.humannamedical.com.br/post/kit-canula-para-exerese-de-calculo-salivar | 3,4 and 6 wires |
| Bougies | Karl Storz, Tuttlingen, Germany | https://www.karlstorz.com/br/pt/search.htm?cat=1000246143 | varying in 3 sizes |
| Conic dilatators | Karl Storz, Tuttlingen, Germany | https://www.karlstorz.com/br/pt/search.htm?cat=1000246143 | unique |
| Dilatator balloons | Humanna medical, Brazil | https://www.humannamedical.com.br/post/kit-canula-para-exerese-de-calculo-salivar | 0.4ml |
| Saline Solution 0.9% | Fresenius Kabi | https://www.fresenius-kabi.com/br | 100ml |
| Salivary probes | Karl Storz, Tuttlingen, Germany | https://www.karlstorz.com/br/pt/search.htm?cat=1000246143 | varying from number 0000 to 6 |
| Sialendoscopes | Karl Storz, Tuttlingen, Germany | https://www.karlstorz.com/br/pt/search.htm?cat=1000246143 | different semi-rigid modular Sialendoscope varying diameter 1.1mm, 1.3 mm, 1.6mm, 1.7 mm |
| Silastic stents | Humanna medical, Brazil | https://www.humannamedical.com.br/post/kit-canula-para-exerese-de-calculo-salivar | varying in number: 4Fr, 6Fr, 8Fr |
| Video Set- Equipment carts and Monitor carts, cables | Karl Storz, Tuttlingen, Germany | https://www.karlstorz.com/br/pt/online-catalog.htm | consisting in Video Monitor, Light xenon 300, Video recorder camera |
References
Reprints and Permissions
Request permission to reuse the text or figures of this JoVE article
Request PermissionThis article has been published
Video Coming Soon
Copyright © 2025 MyJoVE Corporation. All rights reserved