Method Article
Treatment with Locking Intramedullary Nailing for Intertrochanteric Fracture of the Femur Utilizing a New Awl with a Distal Positioner
In This Article
Summary
Here, we present a protocol for accessing the guidewire of intramedullary femoral nailing in obese patients using an in-house designed awl. Using the new awl with a distal positioner for the guidewire insertion and opening the bone can increase efficiency in inserting the guidewire and reduce the difficulty of surgery.
Abstract
Interlocked intramedullary nailing is now established as the preferred method of managing femoral intertrochanteric fractures. Choosing the ideal entry point and inserting the guidewire accurately are key steps of the procedure. Several factors make the procedure more challenging, such as the supine position, obese patients, and the tip of the trochanter not aligning co-linear with the anatomic axis of the femoral medullary canal in the frontal plane. Our team has developed a new awl with a distal positioner that assists the guidewire insertion and entry portal of femurs. This comparative study analyzed 40 intertrochanteric fracture cases treated with locking intramedullary nailing, which were randomized to receive either the new awl incorporating a distal positioner (n = 20) or the conventional guide apparatus (n = 20). Operation time, blood loss, the success rate of the one-time insertion, radiation times, and bone healing time were recorded. The patients (21 males and 19 females) were treated with Gamma 3 and proximal femur nail antirotation (PFNA) with the help of the new awl with a distal positioner or conventional guide apparatus. There were no transoperative complications in the two groups. The surgical time in the new guide apparatus group was significantly shorter compared to the control group. The new awl group achieved a 100% success rate for one-time needle insertion, surpassing the control group's rate of 66.7%. The fluoroscopy time required for the new awl group was obviously shorter compared to that of the control group. However, no significant differences were observed in terms of intraoperative blood loss or bone healing time between the two groups. The newly designed guide awl with a distal positioner could reduce the difficulty in opening the femur for inserting the interlocked intramedullary nail. This tool is especially suitable for obese patients.
Introduction
Epidemiologic studies of hip fractures reported that the number of hip fractures has probably increased significantly in recent years1. Intertrochanteric fracture of the femur as a common hip fracture represents about 31%-35% of all hip fractures2. Interlocked intramedullary nailing is now established as the preferred method of managing femoral intertrochanteric fractures, offering superior biomechanical stability compared to extramedullary fixation systems. The proximal femoral nail anti-rotation (PFNA) from Depuy Synthes and Gamma 3 Nail System from Stryker are both commonly used for the treatment of intertrochanteric femur fracture3. However, when using these systems, especially in identifying nail entry points and inserting guidewire, there are always many problems. Before choosing an entry point, the first procedure is to make the hip adduction. However, the consequent issue is that the reduction cannot be maintained or lost. Because of the proximal valgus of the femurs, the orientation of a guidewire tends to be towards the medial femoral wall and will throughout. These problems are particularly acute in obese patients undergoing supine position.
Recent advancements in intramedullary nailing techniques have underscored the pivotal role of accurate entry-point localization for achieving optimal reduction and stability in intertrochanteric fractures. Conventional entry devices, such as standard awls or guidewire systems, frequently encounter challenges in maintaining alignment due to anatomical variations, proximal femoral valgus deformity, and soft tissue interference, especially in obese patients. Research highlights that improper guidewire placement significantly elevates the risk of medial cortical perforation, delayed union, and implant failure, with error rates surpassing 15% in cases involving osteoporotic bone or complex fracture patterns4. While current solutions, such as fluoroscopy-assisted navigation and adjustable targeting sleeves, partially mitigate these issues, they often necessitate prolonged radiation exposure or complex surgical procedures.
We designed a new awl with a distal positioner, which minimized guidewire malposition and preserved reduction stability during hip adduction. In the below protocol, the details of the new awl and the procedure are described. We used a proximal femoral intramedullary nail to treat the 40 patients with intertrochanteric femur fractures. In this study, 20 patients underwent the procedure with the help of the newly designed guider. As a comparison, the remaining patients underwent the surgery with the help of the regular guide apparatus.
Protocol
The clinical application of this new apparatus has been approved by the Ethics Committee of Tongji Hospital, Tongji Medical College, Huazhong University of Science & Technology. The newly designed guide apparatus is shown in Figure 1. The guide apparatus consists of several parts, including an excellent grip handle, a cannulated curved awl that can insert a 3 mm guidewire, a hammering point, and the distal positioner. The guidewire passing through the awl will deviate 15°-20° to the lateral of the trunk, increasing the operating space.
1. Preparation
- Patient position: Position the patient supine on a radiolucent table. Position the contralateral limb in an adjustable leg holder. Abduct the torso 10°-15° to allow clear access to the intramedullary canal.
- Image intensifier position: Position the image intensifier (G-arm) in the ipsilateral to obtain both anterior-posterior and lateral projections.
2. Operational procedure
- Fracture reduction: Maintain traction and internal rotation of the ipsilateral leg under image intensifier control.
- Drape the patient for the standard femoral nail procedure. Disinfect the surgical field with iodine povidone, extending longitudinally from the costal margin to the foot and transversely from the anterior midline beyond the posterior spine.
- Position four sterile towels strategically.
- Cover the posterolateral hip with the first, the inguinal region with the second, and wrap the anterior and lateral thigh with the third and fourth, securing them with towel clips or adhesive drapes.
- Extend the sterile field with middle sheets, then center a large fenestrated drape over the hip while encapsulating the distal limb using a sterile stockinette and elastic bandage.
- Make a longitudinal skin incision approximately 3-5 cm in length, placing it 2-3 cm proximal to the trochanteric apex and extending along the axis of the femoral shaft. Dissect the gluteus medius fascia. Palpate the tip of the greater trochanter.
- Choose an ideal entry point at the tip of the greater trochanter. Under anteroposterior (AP) fluoroscopy, align the entry point with the trochanteric tip; under lateral fluoroscopy, confirm axial alignment with the medullary canal by centering the entry point within the trochanteric profile.
- Place the awl's tip at the ideal entry point. Then make a small incision at the site of the distal position tube and insert a customized 3 mm wire through the tube. Confirm the tip of the K-wire positioning along the lateral of the femur.
- Advance the customized wire to the correct depth to offset the valgus of the proximal femur. Under the A-P view and lateral view, confirm the extension of the tip of the awl and the continuation of the femoral medullary cavity.
- Insert a 2.5 mm diameter guidewire through the tube of the awl into the femoral medullary cavity with a depth of approximately 15 cm. Check the position of the guidewire under the image intensifier.
- Turn and push or tap gently with a hammer to open the proximal cortex, keeping the tip of the awl at the level of the lesser trochanter during the process.
- Attach the intramedullary nail to the insertion handle using its threaded proximal locking mechanism. Align the nail's proximal end with the handle's coupling interface and secure the connection by tightening it with a torque-limiting wrench.
- Insert the intramedullary nail while aligning its proximal end flush with the greater trochanter tip and terminating the distal end at the metaphyseal-diaphyseal junction of the femoral shaft, maintaining a 10-20 mm gap proximal to the femoral condyles.
- Verify fracture reduction and the proximal locking position under the image intensifier. Assemble the aiming arm to the handle.
- Insert the guidewire and verify nail depth and position for the helical blade or screw. After inserting the proximal blade or screw, complete the distal locking.
3. Post-operation
- Define operative duration as the interval between the initial skin incision and the final dressing application. Record total fluoroscopy time in seconds using the G-arm machines.
- Document the success rate of one-time insertion of the guidewire from the surgical records for analysis.
- Obtain radiographs every 3-4 weeks until the bone healing is achieved and judge through the radiographic criteria of fracture healing5.
Results
Cohort demographics
Between June 2020 and February 2023, 40 patients (21 males and 19 females) with a mean age of 52 years (range 20-63) were admitted to Tongji Hospital with intertrochanteric femur fractures. The patients were treated with locking intramedullary nailing with the help of a newly designed guide apparatus or conventional guide apparatus. Based on the guide apparatus used during the operation, the patients were divided into two groups: the control group (n = 20) and the new guide apparatus group (n = 20). The patients over 60 years old (≥60) were treated with PFNA, and the patients under 60 years old (<60) were treated with the Gamma 3 nail system. The clinical application of this new apparatus has been approved by the Ethics Committee of Huazhong University and conducted in accordance with the Helsinki Declaration of 1975, as revised in 2013. All patients have signed an informed consent form. The demographic characteristics are presented in Table 1. We observed no differences in the data between the two groups.
Results of postoperative clinical and radiographic evaluation
The mean operation time in the newly designed guide group was 45.8 ± 1.6 min, which was less compared to the mean operation time in the conventional guide group, which was 58.0 ± 2.3 min. The intraoperative blood loss in the newly designed guide group was 104.3 ± 5.8 mL, and in the control group, it was 122.8 ± 7.2 mL. There is no significant change between the two groups. The success rate of the one-time inserted guide wire is 100% in the newly designed guide group. In the control group, the success rate was 66.7%. The radiation times were less for the newly designed guide group (14.9 ± 0.7) than for the control group (19.5 ± 0.9). There is no significant change in bone healing time between the two groups. All data are shown in Table 2.
The intraoperative efficacy of the new guide apparatus is systematically demonstrated in Figure 2 and Figure 3. Figure 2 illustrates the critical procedural workflow for femoral medullary access. The distal positioner component facilitated optimal guidewire trajectory alignment through the greater trochanter tip into the medullary canal, effectively reducing cortical perforation risks (Figure 2A,B). Controlled trochanteric entry was achieved by gentle hammer percussion at the predefined entry point (Figure 2C), followed by comprehensive multiplanar verification of implant positioning via intraoperative fluoroscopy (Figure 2D).
Figure 3 documents the clinical implementation of this system in a 56-year-old male with a right intertrochanteric fracture. Preoperative imaging confirmed fracture morphology (Figure 3A), while traction-assisted reduction under fluoroscopic guidance achieved anatomical congruity (Figure 3B). The guide apparatus enabled precise trochanteric entry point localization (Figure 3C) and controlled cortical fenestration using the integrated impactor (Figure 3D). Post-implantation radiographs confirmed appropriate intramedullary nail positioning in both coronal and sagittal planes (Figure 3E). Importantly, 14-month follow-up imaging (Figure 3F) demonstrated uneventful fracture consolidation and successful hardware removal, validating the system's long-term biocompatibility and procedural reproducibility.
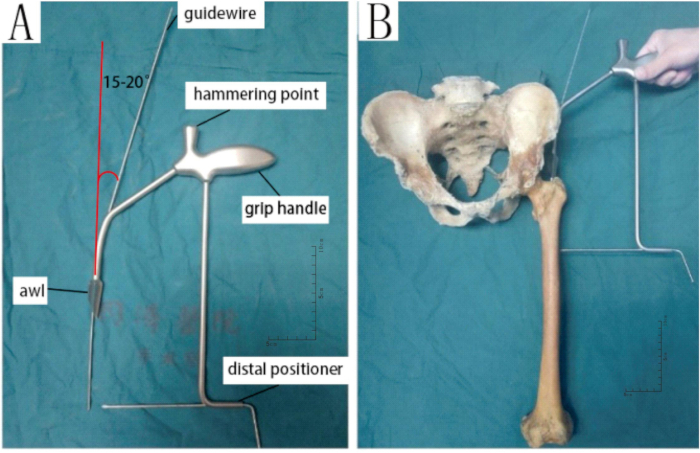
Figure 1: Schematic diagram of the new awl with a distal positioner. (A) The guide apparatus contains several parts, and guidewires were inserted. (B)A femur model is used to show how the guide apparatus works during the operation. The guidewire passing through the awl will deviate 15°-20° to the lateral of the trunk, increasing the operating space. The distal positioner can be inserted into the customed K-wire and positioned in the middle of the anterior and posterior margins of the femur on the lateral cortex. Ensure that the customized wire is inserted to the correct depth, which is a decisive factor in offsetting the valgus of the proximal femur. Please click here to view a larger version of this figure.
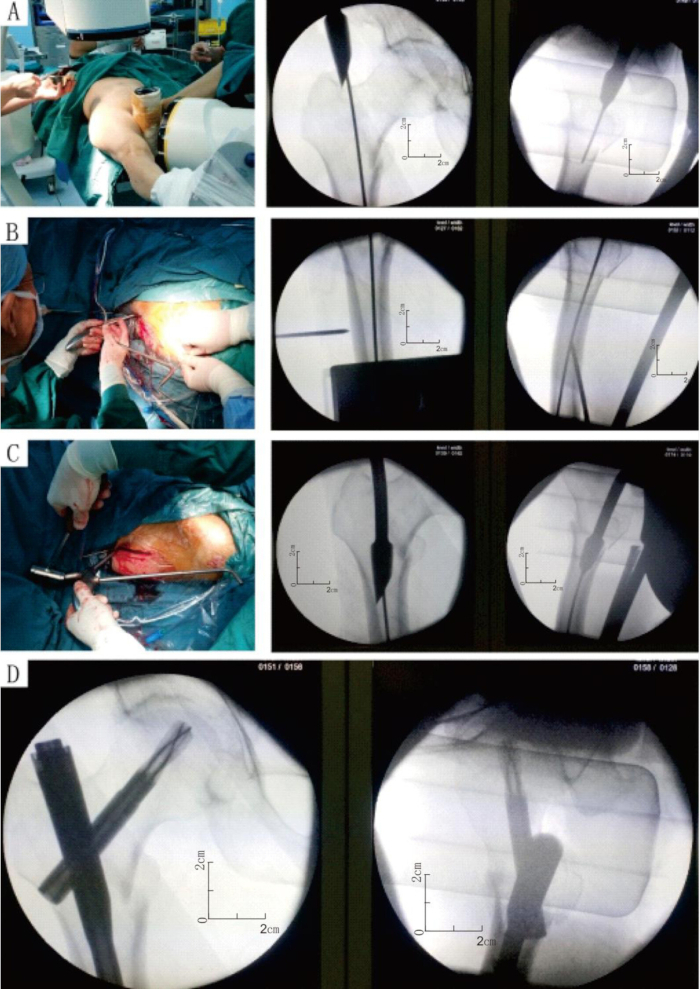
Figure 2: Intraoperative application of the newly designed guide apparatus. (A,B) With the help of the distal positioner of the guide, the guidewire was inserted through the tip of the greater trochanter into the femur medullary cavity safely and effectively. (C) The hammering point was tapped gently with a hammer to open the tip of the greater trochanter easily. (D) Both anteroposterior (A-P) and lateral views of the internal fixation were checked. Please click here to view a larger version of this figure.
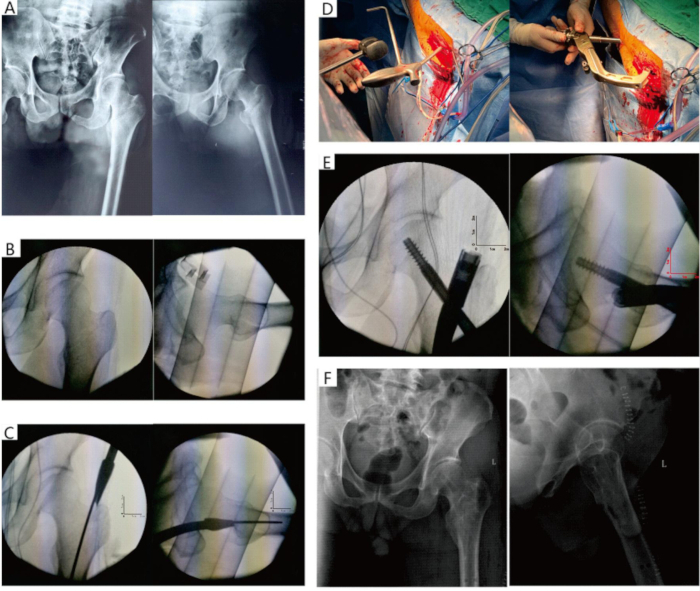
Figure 3: Preoperative, intraoperative, and postoperative X-rays of a 56-year-old man with a right intertrochanteric fracture treated surgically with the newly designed guide apparatus. (A) A 56-year-old man was admitted with a right Intertrochanteric fracture of the femur. (B) Persistent traction and internal rotation of the ipsilateral help complete fracture reduction. The A-P and lateral images of the G arm X-ray. (C) The guidewire was inserted through the tip of the awl into the femur medullary cavity. (D) Intraoperative application of the newly designed guide awl. The hammering point was tapped gently with a hammer to open the tip of the greater trochanter, then inserted the nail. (E) Both anteroposterior and lateral views of the internal fixation were checked. (F) The internal fixation was removed at the request of the patient 14 months later. Please click here to view a larger version of this figure.
| Parameter | Control group | New guide group | P value |
| Patients | |||
| Number | 20 | 20 | |
| Male | 11 | 10 | 0.7524# |
| Side (left) | 9 | 10 | 1.0000# |
| Mean age (years) | 52.7 ± 2.7 | 52.1 ± 2.44 | 0.8688* |
| Age ≥ 60 years old | 6 | 6 | 1.0000# |
| Mechanism of injury | 0.3598# | ||
| Fall injury | 2 | 5 | |
| Car accident | 12 | 9 | |
| Motorbike accident | 1 | 3 | |
| Other injury | 5 | 3 | |
| AO classification | 0.4589# | ||
| 31A1.2 | 10 | 12 | |
| 31A1.3 | 7 | 6 | |
| 31A2.2 | 2 | 0 | |
| 31A2.3 | 1 | 2 |
Table 1: Patients' data overview. # Data were compared using chi-square and Fisher's exact tests; *data were compared using Student's t-test.
| Parameter | Control group | New guide group | P value |
| Mean operation time (min) | 58.0 ± 2.3 | 45.8 ± 1.6* | 0.0001 |
| Blood loss (mL) | 122.8 ± 7.2 | 104.3 ± 5.8 | 0.0541 |
| Success rate of the one-time insertion | 66.70% | 100% | |
| Radiation times (times) | 19.5 ± 0.9 | 14.9 ± 0.7* | 0.0002 |
| Bone healing time (weeks) | 16.8 ± 0.9 | 15.9 ± 0.8 | 0.4389 |
Table 2: Comparison of the operation time, blood loss, radiation times, the success rate of one-time insertion, and bone healing time between the two groups. * P﹤0.05, compared to the control group.
Discussion
The intertrochanteric of the femur is an important pillar for weight bearing through the skeletal system. The area is prone to fractures due to high-level trauma in the young and trivial trauma in the elderly. The principle in the management of intertrochanteric fractures is a good reduction and strong internal fixation. The options contain extramedullary and intramedullary fixation6,7. For stable intertrochanteric fractures, both fixation devices benefited the patients, but extramedullary fixation is better8. Also, this is controversial9. In patients with unstable fractures, the intramedullary fixation is safe and effective compared with the extramedullary fixation10,11. Therefore, intramedullary fixation was generally preferred in patients with intertrochanteric fractures. The present intramedullary fixation devices mainly include PFN, Gamma nail, and PFNA. This study chose Gamma nail and PFNA, which gained great outcomes in intertrochanteric fracture patients as reported in the previous study12.
When the surgeon operated on the patients with intramedullary fixation, there were some problems that needed to be solved in opening the tip of the greater intertrochanteric of the femur. There are three main problems, which are listed here: (1) Insufficient operating space when inserting the guidewire. Especially obese or strong patients in the supine position, due to the more soft tissue they have compared to the thin patient. Meanwhile, the supine position magnifies the technical difficulties. The increased girth of the thighs and increased flank prominence all make the supine more difficult. Also, with a smaller radian in the regular guide apparatus, there is mostly no space for the surgeon to insert the guidewire13. In some situations, the patient's lower limbs may be in the neutral position, even in the abduction position after reduction. If adducting the limb, the reduction is lost. In this case, there is very little space to insert the guidewire. (2) The guidewire tends to penetrate the medial wall of the femur. The nail is advanced through the entry point, necessitates an implant that accommodates both the medially convex curvature in the proximal femur and the antecurvature of the femoral diaphysis to avoid malreduction; otherwise, it will increase localized cortex stress, cause femoral bursting, and iatrogenic fracture during nail insertion14,15.When the entry point on the greater trochanter is found and the distal registration point uncertain, the guidewire may exit through the medial femoral wall, even the anterior wall, and the posterior wall. It is dangerous for the guidewire out of the femur wall, injuring the nerve and blood vessels and causing serious complications. (3) When using the drill bit over the guidewire and through the protection sleeve to open the canal, the surgeon must push the handle of the protection sleeve inwards to keep the drill in line with the medullary cavity of the femur. The handle is difficult to push due to hip obstruction in obese patients. Furthermore, osteoporosis on the lateral aspect of the greater or lateral wall incompetent fracture unconsciously makes the proximal femur canal more lateral.
Due to the problem, our team has designed a new cannulated awl. The design principle of the awl is solving the problems that we encountered during the operation. We acquired a large space to insert the guidewire by increasing the radian and length of the puncture head and the puncture rod. It is easy to insert the guidewire even without hip adduction because of the radian that matches the medially convex curvature (Figure 1). The new guide has a distal positioner, which helps to make sure the guidewire is inserted into the bone cavity. The distance between the tip of the customed wire inserted by the distal positioner and the horizontal guidewire is about 1-2 cm, ensuring that the guidewire is in the medullary cavity and avoiding puncture of the medial cortex. It is effective in increasing the success rate of one-time insertion of the guidewire. We designed the guide with a big handle and a hammering point, which help the surgeon hold the guide easily and open the greater trochanter effortlessly by hammering the hammering point. In cases of comminuted greater trochanter fractures, this protocol involves preliminary anatomical reduction and stabilization of the fracture fragments prior to awl insertion. This is achieved through a combination of Kirschner wire (K-wire) temporary fixation and precise application of pointed reduction forceps. The concave tip configuration of the awl facilitates optimal engagement with the pre-reduced cortical surface. At the same time, its integrated cannulated design permits controlled advancement along a pre-inserted 2.5 mm K-wire trajectory. This dual fixation mechanism combining cortical surface interlock with intramedullary wire guidance effectively mitigates the risk of lateral migration into existing fracture lines.
The potential risk of guidewire deviation into the profunda femoral artery during proximal femoral procedures represents a well-recognized anatomical challenge, particularly at the bifurcation of the femoral artery. While this complication remains a concern in conventional techniques, our redesigned cannulated awl incorporates specific features to effectively mitigate this risk. First, the enhanced curvature of the puncture head and rod aligns more precisely with the natural anatomy of the femoral neck and medullary cavity, facilitating anterograde advancement of the guidewire along the central axis of the femoral neck. This alignment reduces lateral deviation and minimizes the likelihood of medial cortical perforation or inadvertent entry into the profunda femoral artery. Second, the distal positioner serves a dual function: it ensures accurate intramedullary placement of the guidewire while providing tactile feedback during insertion. By maintaining a 1-2 cm safety margin between the guidewire tip and the medial cortex, the device establishes a "protected trajectory" that respects the anatomical boundaries of the femoral canal. Such spatial control is essential for preventing a medial cortical breach, which could otherwise direct the guidewire toward the profunda femoral artery. Furthermore, the ergonomic design enables surgeons to achieve optimal hip positioning (e.g., neutral or slight abduction) without compromising the precision of guidewire placement. This contrasts with traditional methods, which often necessitate exaggerated hip adduction to avoid vascular structures-a maneuver that may inadvertently increase tension on the profunda femoral artery.
McKee and Waddell13 reported on closed intramedullary nailing in a group of morbidly obese patients with particular emphasis on intraoperative techniques. Two of seven patients suffered a fracture of the great trochanter during reaming and insertion of the nail due to the difficulty arising from the prominence of the buttock and flan adipose tissue and adducting the patients' legs on the fracture table. They thought these problems might be less significant due to the lateral positioning of the patients.
In our experience, for patients with pelvic fractures or thoracic and abdominal injuries that preclude lateral decubitus, opening the greater trochanter cortex is particularly difficult. There is only one opportunity, and repeated operations can lead to fracture at the entry point. Tucker et al.16 conducted a multi-center analysis of 151 femoral shaft fracture cases treated with intramedullary nailing procedures at four Level 1 trauma centers. The cohort was stratified by body mass index, with 32 patients (BMI ≥30) categorized as the obese group and 119 patients (BMI < 30) designated as the non-obese group. Notably, their investigation demonstrated significantly extended operative times and increased radiation exposure durations in the obese population undergoing antegrade nailing versus non-obese controls. Another study evaluated the therapeutic efficacy of antegrade femoral nailing in 12 lipodystrophy cases presenting with acute fractures and nonunions17. The inclusion criteria required either a confirmed trochanteric lipodystrophy diagnosis or a body mass index (BMI) ≥ 27. All surgical interventions were conducted with patients maintained in the supine position, utilizing a standardized piriformis fossa approach as the initial entry portal. Intraoperative imaging consistently demonstrated critical deviations of guidewire trajectories exceeding acceptable angulation, with pronounced medial displacement toward the lesser trochanter. Ostrum's technical modification involving lateral displacement to the greater trochanteric apex significantly improved trajectory accuracy. Biomechanical analysis indicates that minor variations in entry point selection combined with implant dimensional characteristics may precipitate angular deformities at the fracture interface. Specifically, lateralized entry portals were correlated with iatrogenic varus malpositioning, necessitating strict avoidance of this approach18.
The use of the newly designed guide apparatus to guide the guidewire insertion and opening of the bone provided high accuracy, with a short operative time and a few radiation times. The success rate of one-time insertion data is 100%. Radiation exposure during the operation is a concern for both the surgeon and the patient. Low radiation exposure by using the designed guide apparatus benefits both the surgeon and the patient.
Although this series consists of a few numbers of patients, we believe the new guide we used is safe and accurate for insertion of the guide wire.
Disclosures
The authors declare that they have no competing interests.
Acknowledgements
None
Materials
| Name | Company | Catalog Number | Comments |
| Awl with a distal positioner | In house | N/A | The awl is to guide wire insertion and open the femoral bone. |
| Gamma3 system | Stryker | 603611 | The Gamma3 System is intended to achieve functionally stable osteosyntheses and stabilization of bones and bone fragments |
| Hip joint surgical instrument set | Shanghai Jinzhong Surgical Instruments Co., Ltd. | P24020 | The hip joint surgical instrument set is to facilitate surgical procedures involving locked intramedullary nailing for the treatment of intertrochanteric femoral fractures. |
| Image intensifier (G-arm) | Swemac imaging | 04-7100020A | The image intensifier (G-arm) is to obtain both anterior-posterior and lateral projections. |
| Iodine povidone | Wuhan Operation Fine Chemical Co.,Ltd | WYH001 | Iodine povidone is to disinfect the surgical field. |
| PFNA | DePuy Synthes | 04.045.870S | PFNA permits an intramedullary approach for the fixation of fractures of the femur. |
References
Reprints and Permissions
Request permission to reuse the text or figures of this JoVE article
Request PermissionExplore More Articles
This article has been published
Video Coming Soon
Copyright © 2025 MyJoVE Corporation. All rights reserved